Rev Cuid. 2021;12(2):e1165
http://dx.doi.org/10.15649/cuidarte.1165
RESEARCH ARTICLE
Cardiovascular Risk and Factors Associated to the Health in Hypertensive African Descent People Resident in Quilombola Community
Riesgo cardiovascular y factores asociados a la salud en personas afrodescendientes hipertensas residentes en la comunidad Quilombola
Risco cardiovascular e fatores associados à saúde em pessoas afrodescendentes hipertensas residentes em comunidade Quilombola
Randson Souza Rosa1, Ícaro José do Santos Ribeiro2, Jaine Kareny da Silva3, Luiz Humberto Rodrigues Souza4, Diego Pires Cruz5, Rudson Oliveira Damasceno6, Edison Vitório de Souza Junior 7, Rita Narriman Silva de Oliveira Boery8
History
Received:: 24th March 2020
Accepted: 2th Febrary 2021
Published: 24th May 2021
How to cite this article : Rosa, Randson Souza; Ribeiro, Ícaro José do Santos; Silva, Jaine Kareny da; Souza, Luiz Humberto Rodrigues; Cruz, Diego Pires; Damasceno, Rudson Oliveira; Souza Júnior, Edison Vitório de; Boery, Rita Narriman Silva de Oliveira. Cardiovascular Risk and Factors Associated to the Health of Hypertensive African Descent People Resident in Quilombola Community. Revista Cuidarte. 2021;12(2):e1165. http://dx.doi.org/10.15649/cuidarte.1165
![]() Atribución 4.0 Internacional (CC BY 4.0)
Atribución 4.0 Internacional (CC BY 4.0)
Abstract
Introduction: Hypertension is a cardiovascular risk factor of wide magnitude among people of African descent, especially those living in Quilombos. However, little is known about the factors associated with cardiovascular risk in residents of the urban Quilombola community. Objetive: To analyze the cardiovascular risk and health-related factors in the family context of hypertensive Afro-descendants living in an urban Quilombola. Materials and methods: It is a cross-sectional and community-based study carried out from November 2017 to March 2018. The study’s population consisted of 303 hypertensive patients enrolled in the family health unit, with ages ranging from 35 to 79 years old, of both genders; and using antihypertensive drugs. The instruments used for data production were: The Primary Arterial Hypertension Questionnaire and the Framingham Risk Score. Results: There was a significant association between cardiovascular risk and cardiovascular disease (CVD) family history (p<0.011), type II diabetes (p<0.001) and overweight and obesity (p<0.010). Conclusion. Research has shown that hypertensive Quilombola people have consistent cardiovascular risk outcomes, especially with CVD family history, type II diabetes, overweight and obesity, schooling and gender with significant associations.
Keywords: Cardiovascular Disorders; Risk Factors; African Continental Ancestry Group; Vulnerability in Health.
Resumen
Introducción: La hipertensión es un factor de riesgo cardiovascular de gran magnitud entre las personas de ascendencia africana, especialmente las que viven en quilombos. Sin embargo, se sabe poco sobre los factores asociados con el riesgo cardiovascular en los residentes de la comunidad urbana Quilombola. Objetivo: Analizar el riesgo cardiovascular y los factores asociados con la salud en el contexto familiar de los descendientes africanos hipertensos que viven en una comunidad urbana de Quilombolas.Material y métodos: Este es un estudio transversal y basado en la comunidad, realizado desde noviembre de 2017 hasta marzo de 2018. La población de estudio consistió en 303 pacientes hipertensos inscritos en la unidad de salud familiar, de edad de 35 a 79 años, ambos sexos; y en el uso medicamentos antihipertensivos. Los instrumentos utilizados para producir los datos fueron: el Cuestionario de Hipertensión en Atención Primaria, la puntuación de riesgo de Framingham. Resultados: Se observó una asociación significativa entre el riesgo cardiovascular y los antecedentes familiares de enfermedad cardiovascular (ECV) (p <0.011), diabetes tipo II (p <0.001) y sobrepeso y obesidad (p <0.010). Conclusión: La investigación mostró que las personas Quilombolas hipertensos tienen resultados consistentes con respecto al riesgo cardiovascular, especialmente con la inclusión de antecedentes familiares de ECV, diabetes tipo II, sobrepeso y obesidad, educación y sexo con asociaciones significativas.
Palabras clave: Enfermedades cardiovasculares; Factores de riesgo; Grupo de ascendencia continental africana; Vulnerabilidad de salud
Resumo
Introdução: A hipertensão é um fator de risco cardiovascular de ampla magnitude entre pessoas de ascendência africana, principalmente, as que vivem em Quilombos. No entanto, pouco se sabe sobre os fatores associados ao risco cardiovascular em residentes na comunidade Quilombola urbana. Objetivo: Analisar o risco cardiovascular e fatores associados à saúde no contexto familiar de descendentes africanos hipertensos que vivem em uma comunidade Quilombola urbana. Material e métodos: Trata-se de um estudo censitário de base comunitária, realizado de novembro de 2017 a março de 2018. A população do estudo foi composta por 303 pacientes hipertensos matriculados na unidade de saúde da família, com idades entre 35 e 79 anos, ambos os sexos; e em uso de medicamentos anti-hipertensivos. Os instrumentos utilizados para produzir os dados foram: o Questionário de Hipertensão na Atenção Primária, e o escore de risco de Framingham. Resultados: Foi observada associação significativa entre risco cardiovascular e histórico familiar de doença cardiovascular (DCV) (p <0,011), diabetes tipo II (p <0,001) e sobrepeso e obesidade (p <0,010). Conclusão: A pesquisa mostrou que pessoas hipertensas quilombolas apresentam resultados consistentes em relação ao risco cardiovascular, principalmente com a inclusão de histórico familiar de DCV, diabetes tipo II, sobrepeso e obesidade, educação e sexo com associações significativas.
Palavras-chave: Doenças cardiovasculares; Fatores de risco; Grupo de ascendência continental africana; Vulnerabilidade à saúde.
Introduction
In Brazil, Quilombola populations are conceptualized in the context of ethnic minority groups belonging to the black population1, which includes people with black, brown, indigenous and white (uncommon) skin color. They are mostly residents of rural or semi-urban areas, and a minority live in urban areas, where together they make up a representative part of the Afro-Brazilian population, and at the same time, are forgotten by the society.
Afro-descendants living in these communities share in their daily living and health conditions, knowledge, attitudes, beliefs, cultures and alternative health practices that are inherited from their ancestors. These facts put them in the spotlight in the health research context, since they live in social vulnerability conditions and, at times, are distant from healthcare service networks, which hinder their access to diagnostic, clinical, therapeutic and health rehabilitation services, thus potentiating chronic illness due to conditions that are sensitive to the promotion, prevention and control of cardiovascular diseases (CVDs).
The complexity related to the etiology of cardiovascular diseases is marked by genetic, social, cultural, economic aspects2, of CVD’s premature history in the family3, behavioral risk factors expressed by unhealthy diet, alcohol and tobacco abuse, physical inactivity, overweight, stress, hypercholesterolemia, Diabetes Mellitus and Systemic Arterial Hypertension (SAH) itself4.
It is worth noting that men are affected by CVDs earlier in life when compared to women, and that the skin color/race, in black, brown or white people and included in the age group below 70 years old are considered as factors that increase vulnerability to falling sick due to this chronic deteriorating health5.
Studies conducted in the USA show that African-American populations have a higher incidence and risk for premature death due to Coronary Artery Disease (CAD) compared to their general population 6-8, and attribute such data, especially, to the influence of social determinants. It should be noted that African Americans live under conditions of chronic, family, economic, social and cultural vulnerability, and have the same ancestry origin of the Quilombolas belonging to the Brazilian communities.
Multiethnic studies that have assessed risk in socially vulnerable populations are still incipient, mainly due to studies that have analyzed the influence of social determinants on health in hypertensive Quilombolas in urban areas. Understanding this relationship can enable health promotion, prevention of health problems, adequate treatments, changes in inappropriate behaviors, as well as the improvement of harmful health conditions deleterious that affect the system cardiovascular disease, which can cause negative clinical impacts on health and quality of life in the ethnic-racial group under study and in those with similar characteristics.
Therefore, this study’s objective was to analyze the cardiovascular risk and the factors associated with the health of hypertensive Afro-descendants resident in an urban Quilombola community.
Materials and Methods
Study design and period
It is a cross-sectional, community-based census study carried out between November 2017 and March 2018.
Study population and eligibility criteria
Based on the total population ((N=483), an epidemiological census was carried out in the family history files, belonging to the Family Health Unit (FHU), and the interviewees were organized by census sectors, according to the micro areas existing in the community.
The research adhered to the following inclusion criteria: (1) People living in Barro Preto community; (2) registered at the FHU; (3) between 35 and 79 years old; (4) both genders; (5) diagnosed with hypertension; and (6) on antihypertensive treatment. Exclusion criteria were people with a CVD diagnosis; (2) with physical, mental or emotional impairment; (3) not found at the time of the interview, at different days and times; and (4) did not attend the blood collect stage of the study.
Of the 400 eligible individuals with the potential to participate in the survey, 21 people were not found in their homes, and 4 moved to another address. Thus, 375 hypertensive individuals living in the community households were interviewed, who met the research’s inclusion and exclusion criteria. However, 68 were excluded because they did not attend the blood collect, and 4 had incomplete questionnaires, resulting in 303 people for analyzing this study.
Data collection and ethical aspects
Data collect took place in two stages: clinical evaluation with questionnaire completion, body composition assessment and blood pressure (BP) at the time of the interview in the participants' homes. The other stage corresponded to venous blood collect at the Family Health Unit (FHU), located in the study community.
The instruments used that were validated at the national level were: SAH in Primary Health Care (PHC)9 and the Framingham Risk Score, FRS. FRS had consistent and important outcomes for preventing and controlling cardiovascular diseases in a study with African-Americans in the Framingham study10. FRS assesses the risk on developing acute myocardial heart attack over an estimated 10 years in individuals who have not undergone coronary events and can classify individuals with low risk (<10%), intermediate risk (10-20%), and high risk (>20%)11.
In the clinical evaluation on body composition, weight, height, BMI and waist circumference the procedures adopted and performed were those in accord to the technical instructions stated in the anthropometry manual of the National Health Survey (NHS) 12. In order to obtain people's body mass (in kilograms/kg), this was measured using a digital bio-impedance scale, Omron branded body control (HBF-514C model), with a maximum capacity of up to 150 kg. Stature (in centimeters, cm) was verified through a personal portable Sanny® stadiometer caprice (model ES2060).
Waist circumference (WC) (in centimeters, cm) was measured using an inelastic and extensible Sanny® measuring tape (model SN-4010), with WC cut-off points ≥ 102 cm in men and CC ≥ 88 cm in women, according to the criteria of the National Cholesterol Education Program III (NCEP III) 13.
Body Mass Index, BMI (in kg/m2) was obtained by the cut-off point recommended by the World Health Organization, using the following formula: division of body mass by squared height, (BMI = weight/height2) considering participants as being overweighed (overweight and obesity) with BMI ≥ 25 kg/m2 and eutrophic with BMI <2 5 kg/m.2, 14
Blood pressure (BP) was measured using an Omron® digital sphygmomanometer (HEM-7113 model), and the values of systolic (SBP) and diastolic blood pressure (DBP) were obtained according to the recommendations of the VII Brazilian Hypertension Guidelines published by the Brazilian Hypertension Society15.
The study was submitted and approved by the Research Ethics Committee of Faculdade Independente do Nordeste - FAINOR, opinion No.: 2.015.327 e CAAE No.: 66705617.2.0000.5578.
Data analysis
Categorical variables were presented in absolute and relative frequency, and the differences among the groups with and without cardiovascular risk were tested using the chi-square test. Variables that displayed a p value < 0.2 were introduced in a multivariate logistic regression model, backward method, looking for the best model fit. Data was analyzed using the Statistical Package for Social Sciences - SPSS for Windows software, version 21.0, with a significance level of p < 0.05.
Results
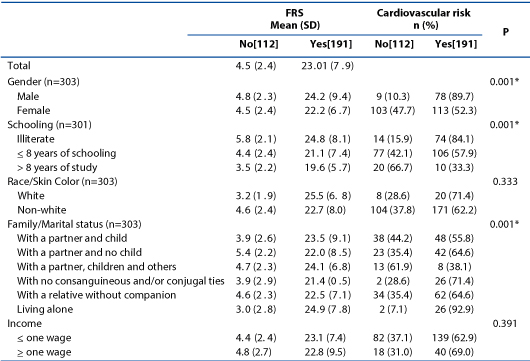
Of the 303 hypertensive individuals living in the Quilombola community who met the study eligibility criteria, mean age was 59.8 years old. (11,3) Cardiovascular risk prevalence (moderate and severe) was 63% (191). Among the hypertensive patients evaluated with cardiovascular risk, it was more prevalent in the following categories of socio-demographic variables: 52.3% (113) in women, 57.9% (106) with less than eight years of schooling, 84.1% (74) reported being illiterate, 62.2% (171) were included in the subgroup of non-whites (brown, black and indigenous), 64.6% (62) lived with relatives and without a partner, of which 62.9% (139) with economic income less than or equal to one minimum wage, according to the characterization in Table 1.
Table 1. Socio-demographic characteristics of hypertensive Afro-descendants resident in Quilombola community, according to cardiovascular risk stratification. Jequié, 2018. (N= 303).
Significant analyses for the cardiovascular risk stratification are described in Table 2, showing 55% (N=93) of hypertensive patients with a CVD family history, (p<0.011) 87.3% (N=62) with type II diabetes (p<0.000) and 59.3% (N=137) with overweight and obesity (p<0.010). Other attenuating and aggravating data were also noted in the participants, but were not associated with cardiovascular risk, of which 61.5% (N=169) did not smoke, 63.5% (N=158) did not report using alcohol and 64.1 (N=98) did not practice physical activity (Table 2).
Table 2. Health profile and life habits of hypertensive Afro-descendants resident in Quilombola community, according to cardiovascular risk stratification. Jequié, 2018. (N= 303)

The multivariate analysis started from a saturation model composed of the variables that presented p <0.2 in the bivariate analyzes. Using the backward method, two models were built until reaching the statistically most appropriate (model 3) presented below (Table 3). Male gender (OR 0.032 [95% CI 0.009-0.18]) and in a family/conjugal situation “With a partner/children/others” (OR 0.074 [95% CI 0.009- 0.637]) have a protective factors. On the other hand, risk factors were pointed out as being illiterate (OR 12.729 [CI95% 2.890-56.057]) end being affected by Type 2 DM (OR 7.249 [CI95% 2.788-18.846]).
Table 3. Gross and adjusted Odds Ratio (OR) and 95% confidence interval for the final regression model. Jequié, 2018. (N= 303)
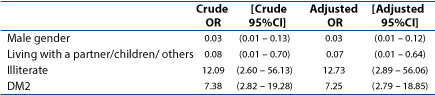
*Hosmer-Lemeshow (p>0.05)
Discussion
The increased burden of CVDs in semi-urban communities in developing countries, as in most African countries, shows factors associated with the overlapping prevalence of cardiovascular risk factors, which usually show insidious, an asymptomatic origin and barriers to early diagnosis and risk-related management optimization16. It is important to discuss the grouping of health indicators related to excess risk in the context of ethnic health inequalities, in order to elucidate health needs due to inequalities in healthcare accessibility17.
Assessing cardiovascular risk in people requires primary identification of multiple associated factors18. Very often, they include modifiable and non-modifiable risk factors that can have implications on people's health since that the presence of multiple factors may turn CVD prevention unpractical, as well as impair access to healthcare services, such as the performance of a simple laboratory blood test, capable of predicting cardiovascular risk3.
The investigation’s results showed that (63%) of the residents in the investigated community were in the strata of moderate and severe cardiovascular risk, highlighting an increase in the prevalence in the female subgroup. In a cross-sectional study on cardiovascular risk among 750 residents in semi-urban communities in southwestern Nigeria, Africa, cardiovascular risk (moderate and severe) was estimated in (22.9%) of the residents, of whom (70.6 %) corresponded to the female gender, where it can be estimated that about 1 out of 4 had a 10% to 20% chance of developing a cardiovascular event over the next ten years16. In another study, also conducted in Africa, the average risk for developing CVD in the next 10 years was 3.7 ± 5.3% and of moderate and high risk for developing CVD according to FRS, respectively, 11.8% and 1.9%19.
In a multi-ethnic study referred to as Jackson Heart Study (JHS), the largest CVD cohort study among African-Americans conducted in the United States, it was pointed out that people with cardiovascular risk live in unfavorable neighborhoods and have less family income and education20.
Results from an ethnic, sociocultural, cross-sectional study with people living in rural and urban environments in Nigeria, show that income level had no statistically significant relation with the prevalence of the risk factor for CVD21. The results are in line with the study under discussion.
A cross-sectional study carried out in Nigeria, with residents of urban areas, inferred that family composition linked to the number of children and dependents causes reasons for concern and stress among married couples, especially, when compared to unmarried and divorced individuals, and evidenced that hypertension, DM, overweight and obesity, arterial wall thickening, large family size/family dependence, and social activity were cardiovascular risks associated with marital status22.
In a meta-analysis study, it was found that married people had lower mortality rates due to cardiovascular diseases and risk factors due to the protective effect of marriage, since the spouse encouraged their partner in the search for medical help, medication use and health monitoring, as evidenced in married men, as they most often have better health behaviors than unmarried men23.
The findings regarding marital/family situation may be associated with low family income and the permanence of non-protective life-styles of cardiovascular health being adopted, mainly those who live “with a relative and without a partner”, being represented, mainly, by elderly people, widows and retirees and who are sometimes the only providers for the household, where their livelihood is directed only for the subsistence of their family dependents.
In this context, they live in chronic vulnerability conditions, since they cannot afford to finance necessary healthcare such as medical appointments, drug treatment and, often, cannot access primary healthcare services because they do not have the necessary economic standing to pay for their own transport. Consequently, these factors potentiate chronic cardiovascular disease. Those married with children live in conditions similar to the variable “With a relative and without a partner”.
The outcomes of the multivariate analysis corroborate a meta-analysis review, which demonstrated the relationship between married ones to divorced or widowed ones and unmarried ones, where divorced, widowed, and unmarried individuals had a high chance of developing CVD (OR 1.42; 95% CI 1.00 to 2.01) and consequently, developing a premature death24.
In the population-based study conducted in the USA, there were higher mortality rates in single men than in married men after a heart attack event25. In the study under discussion, although unrepresentative results have been found, it is to be considered as an important aggravating factor, since single people are responsible for the protagonism of their own care, like preparing their own nutritional diet, experience the work process, often stressful in their daily life and, when they return home, many live locked in their houses, without any distraction or social interaction and, sometimes, when they experience a process of chronic illness, they delay seeking for specialized help, which worsens their health conditions.
The outcomes from assessing the family history of premature coronary artery disease and cardiovascular risk in Multi-Ethnic Study of Atherosclerosis (MESA)26 corroborate with this study, since a statistical association (p<0.001) was found and recommendations were made for including the family history of premature CAD in risk assessment scores in individuals at high risk to clinical practice, as well as genetic and environmental factors, since cardiovascular diseases on first-degree relatives (parents), can predict cardiovascular events throughout life27, 28. This fact reinforces the need for future research on the genetic determinants of cardiovascular risk on the population’s health.
Non-protective behaviors of cardiovascular health are the main risk factors (physical inactivity, inadequate diet, alcohol use and smoking) found in the society, given the increase in world prevalence due to urbanization29. However, grouping these risk factors increases the chances for people to develop cardiovascular disease, even if presented individually30. A study with Africans from the North West Province of South Africa also found no significance correlation between the clinical variables “alcohol use” and “smoking” 31.
Although the behavioral variables “smoking’’ and “alcohol use’’ were not significantly associated in our study, the findings in this investigation revealed that Quilombola hypertensive people have a lifestyle considered to be protective of cardiovascular health, given that the self-reported variables revealed a high prevalence for the non-use of these substances in people with cardiovascular risk. It can be inferred that the uncontrolled/abusive use of these harmful substances to human cardiovascular health, causes clinical impacts on the health-disease process and cardio-deleterious effects on hypertensive people of African descent.
In this study, community research analyses elucidated a significant association between cardiovascular risk and BMI. The association’s outcome differs from the findings in the study on excess cardiovascular risk in Jamaican men and women, showing results contrary to this study, since it did not find a significant association between the variables of high CVR/BMI32. The hypothesis conceived for non-association is that the surveyed Jamaican black people are experiencing a more labor-intensive working process based on agriculture that requires more physical effort for their subsistence, while this study’s participants live in a typically urban area, where many are unemployed, financially dependent on their relatives, who develop sedentary risk behaviors and with cardio-deleterious effects. The hypothesis can be reinforced since half of those surveyed with cardiovascular risk did not practice physical activity.
In agreement with the study carried out with Jamaican men and women, corroborating data from the study under discussion, since no statistical difference was found regarding physical activity and the risk for 10 years of CVD, according to the FRA, for men and women according to categories in relation to physical activity32. The high rates of obesity among African-Americans are related to insulin resistance frequency and to a 50% increase in DM prevalence33. In an African-Americans study, we found cases with high rates of obesity and risk factors for CVDs, with racial and ethnic disparities being attributed to the fact that CVDs in African-Americans were higher in relation to white people34.
When evaluating family context through the interview, it was not found that FHU health professionals generally seek to know the hypertensive person’s family, with few orienting on lifestyles and treatment for the hypertension condition, nor do they always include relatives in the family treatment.
Family participation throughout the hypertension progression becomes an important clinical care management, which favors changes in lifestyle among people affected by the pathology, and it is important that health professionals include relatives of patients with hypertension in the clinical procedures adopted in order to improve the effectiveness for therapeutic adherence35.
It is known that grouping the history of factors associated with cardiovascular risk increases the risk for CVD36. Thus, the multivariate analysis revealed important protective factors and risk for promoting, preventing and controlling chronic cardiovascular disease in hypertensive Quilombolas. The result highlights the following as protection factors: “being male” and in family/conjugal situation “With a partner/children/others”. It can be inferred that, for the most part, men, as providers of the family, develop in the daily life of their labor process more physical exertion and vigorous activities and are supported by their relatives, in healthcare need situations, behaving like a protective effect for cardiovascular health and attenuating the cardio-deleterious effects that affect men’s cardiovascular system.
This fact was not evidenced in the variables “being illiterate” and “Type 2 DM” being displayed in the final model as non-protective risk factors for cardiovascular health. The risk of developing cardiovascular risk in 10 years was lower among people with higher schooling levels37. The findings regarding the educational variable translate important interpretations for monitoring and evaluating hypertensive people’s health, considering that knowledge on this variable can elucidate ethnic racial disparities in access to health, since more educated people understand better their health-care process, seek medical and health services more frequently and, therefore, the risk for cardiovascular disease and cardiovascular effects will be lower. Likewise, it is capable of translating vulnerability conditions in chronic health, considering that the lower the schooling is, the greater is the risk for cardiovascular disease, and the greater will be the interventions for promoting, preventing and controlling cardiovascular diseases, mainly in the perspective of achieving the rehabilitation of cardiovascular health in hypertensive people living in a Quilombola community or who has suffered a cardiovascular event.
Cardiovascular risk evidenced a significant association with DM, corroborating with the findings in the studies38, 39. DM is closely associated with cardiovascular disease (CVD), since CVD morbidity and mortality are more prevalent in people with diabetes40. In men with diabetes, the relative risk for CVD morbidity and mortality ranges from 1 out of 3 men and, among diabetic women, it varies from 2 out of 5 when compared to people with no DM41.
Studies prove that there are disparities in the development of CVDs in diabetic people in relation to gender, the most prevalent mainly being in the course of life of women, since they suffer deleterious influences even in their reproductive age, with the presence of endocrine disorders like the polycystic ovary syndrome and gestational disorders represented by pre-eclampsia, hypertension and diabetes, which, due to premature onset of menopause, are also important risk factors for CVDs, exclusive to women42, 43.
Diagnosed diabetes is an equivalent risk factor for prior myocardial heart attack44 In a cohort of descendants of the Framingham Heart Study, it was found that African-Americans with higher blood pressure are more likely to develop diabetes than those with normal blood pressure, with an increase in diabetes among hypertensive patients due to the higher adiposity recorded rate, among other cardio-metabolic risk factors45.
This study has limitations in the methodological design adopted, since cross-sectional studies do not establish the causal link for the disease. Future research is needed in this population, as it is an urban Afro-Brazilian Quilombola community, living in different contexts when compared to other Quilombola communities, especially because they experience in their daily lives, constant exposure to low health conditions and typically urban human behavior. This reinforces the need for new longitudinal segment research in order to better understand the relationship between cardiovascular risk and new risk factors associated with health determinants in their social, economic and cultural context.
Conclusion
Research has shown that hypertensive Quilombola people have consistent cardiovascular risk outcomes, especially with CVD family history, Type II diabetes, overweight and obesity, schooling and gender with significant associations and high prevalence. After the gross and adjusted analysis of some variables such as being “male” and “living with a partner/children/others”, they behave as protective effects for cardiovascular health. Whereas the variables “schooling” and having “Type II diabetes” showed a cardio-deleterious effect.
Clinical evaluation on the risk in hypertensive Afro-descendants living in a Quilombola community evidenced that the majority is under cardiovascular risk, and revealed conditions for chronic cardiovascular disease in the studied population, since risk conditions are considered subclinical for both hypertensive individuals and health professionals, that is, they were not known to both. For this reason, arterial hypertension can be considered as a cardio-deleterious disease, with and insidious origin, multifactorial and silent progressive course, capable of causing disastrous consequences on human health.
It can be inferred that using the Framingham score has proved to be a health technology with importance for public health and clinical practice, since it shows individual and collective therapeutic efficacy, capable of evaluating cardiovascular risk through population surveys, with cost-effectiveness and proposing therapeutic measures compatible with hypertensive risk conditions, through pharmacological and non-pharmacological therapeutic measures.
In this perspective, classifying people by risk strata can contribute to the clinical management of health care and to the control of chronic cardiovascular disease in people with hypertension who are at high risk of developing an acute cardiovascular event, as well as causing protective clinical impacts on the health and quality of life of people who suffer from chronic hypertension.
As contributions to clinical practice, it becomes necessary to implement multidisciplinary clinical interventions supported by clinical teaching strategies for patients regarding the knowledge of cardiovascular risk and risk factors with cardio-deleterious effects (physical inactivity, inadequate diet, use of alcohol and smoking), as well as diagnostic measures (laboratory tests) like evaluating, monitoring and tracking clinical parameters on the lipid profile, blood pressure control, glycemic control and risk behavior variables, in order to guarantee comprehensive care and cost -effectiveness of health services in populations of minority groups that experience their health-disease process, low socioeconomic conditions and vulnerability of their cardiovascular health conditions.
Conflict of Interest: The authors have no conflicts of interest to declare.
Source of Funding: None
References