Tahissa Frota Cavalcante1
Raphaella Castro Jansen2
José Erivelton de Souza Maciel Ferreira3
Cristefânia Meirú de Lima4
Huana Carolina Cândido Morais5
Rafaella Pessoa Moreira6

Rev Cuid. 2022; 13(3): e2695
http://dx.doi.org/10.15649/cuidarte.2695
REVIEW ARTICLE
Repercussions of COVID-19 in hemodialysis patients: a systematic review
Repercusiones del COVID-19 en pacientes en hemodiálisis: Una revisión sistemática
Repercussões da COVID-19 em pacientes em hemodiálise: uma revisão sistemática
Tahissa Frota Cavalcante1
Raphaella Castro Jansen2
José Erivelton de Souza Maciel Ferreira3
Cristefânia Meirú de Lima4
Huana Carolina Cândido Morais5
Rafaella Pessoa Moreira6
|
Received: May 17th 2021
Accepted: August 2th 2022
Published: October 6th 2022
How to cite this article: Frota Cavalcante Tahissa, Castro Jansen Raphaella, de Souza Maciel Ferreira José Erivelton, Meiru de Lima Cristefânia, Cândido Morais Huana Carolina, Pessoa Moreira Rafaella. Repercussions of COVID-19 in hemodialysis patients: a systematic review. Revista Cuidarte. 2022;13(3):e2695. http://dx.doi.org/10.15649/cuidarte.2695
Abstract
Introdution: The immunosuppressive state of patients with CKD increases their risk of developing poor clinical outcomes if they acquire COVID-19 infection. Objetive: To identify the scientific evidence about the repercussions of COVID-19 in hemodialysis patients. Materials and méthods: A systematic review was conducted in this study. The databases Cochrane Library, Web of Science, Science Direct, PubMed, and Virtual Health Library were searched to identify relevant studies. The methodological quality of the studies was assessed using the adapted Downs and Black checklist. The review adhered to the PRISMA guidelines. Results:A total of 16 articles were included after the screening process. All articles had a methodological quality higher than 66.8%. The most common repercussions of COVID-19 in hemodialysis patients were the increased mortality rate (75%), development of typical signs and symptoms of the disease such as fever, cough, dyspnea, and fatigue (68.75%), lymphopenia (68.75%), progression to severe acute respiratory syndrome (56.25%), need for mechanical ventilation (50%), and admission to intensive (50%). Conclusión: The hemodialysis patients are more susceptible to COVID-19 infection and, when infected by SARS-CoV-2, these patients have more adverse clinical outcomes, more serious diseases, higher mortality, and worse prognosis than the general population. The repercussions of COVID-19 in hemodialysis patients reveal a need for preventive nursing care in hemodialysis clinics.
Keywords: SARS-CoV-2; COVID-19; Hemodialysis; Renal Insufficiency, Chronic; Nursing.
Resumen
Introducción: El estado de inmunosupresión de los pacientes con enfermedad renal crónica (ERC) aumenta su riesgo de obtener resultados clínicos desfavorables si llegaran a contraer COVID-19. Objetivo: Identificar la evidencia científica acerca de las repercusiones que tiene el COVID-19 en los pacientes en hemodiálisis. Materiales y Métodos: Se realizó una revisión sistemática en este estudio. Se hizo una búsqueda en las bases de datos Cochrane Library, Web of Science, Science Direct, PubMed y Virtual Health Library para identificar estudios relevantes. La calidad metodológica de los estudios se evaluó mediante la lista de chequeo adaptada por Downs y Black. La revisión siguió los lineamientos de la declaración PRISMA. Resultados:Tras el proceso de selección se incluyeron un total de 16 artículos en la revisión. Todos los artículos obtuvieron una calidad metodológica superior a 66,8%. Las repercusiones más comunes del COVID-19 en los pacientes en hemodiálisis fueron el aumento de la tasa de mortalidad (75%), el desarrollo de signos y síntomas típicos de la enfermedad como fiebre, tos, disnea y fatiga (68,75%), linfopenia (68,75%), progresión a un síndrome respiratorio agudo grave (56,25%), necesidad de ventilación mecánica (50%) e ingreso a cuidados intensivos (50%). Conclusiones: Los pacientes en hemodiálisis son más susceptibles a contraer COVID-19 y, cuando contraen el SARS-CoV-2, tienen resultados clínicos más adversos, enfermedades más graves, mayor mortalidad y peor pronóstico que la población general.
Palabras Clave: SARS-CoV-2; COVID-19; Diálisis Renal; Insuficiencia Renal Crónica; Enfermería.
Resumo
Introdução: O estado imunossupressor dos pacientes com CKD aumenta seu risco de desenvolver maus resultados clínicos se eles adquirirem a infecção COVID-19. Objetivo: Identificar as evidências científicas sobre as repercussões da COVID-19 em pacientes com hemodiálise. Materiais e Métodos: Uma revisão sistemática foi conduzida neste estudo. As bases de dados Cochrane Library, Web of Science, Science Direct, PubMed e Virtual Health Library foram pesquisadas para identificar estudos relevantes. A qualidade metodológica dos estudos foi avaliada utilizando a lista de verificação Downs e Black adaptada. A revisão seguiu as diretrizes do PRISMA. Resultados: Um total de 16 artigos foram incluídos após o processo de triagem. Todos os artigos tinham uma qualidade metodológica superior a 66,8%. As repercussões mais comuns da COVID-19 em pacientes de hemodiálise foram o aumento da taxa de mortalidade (75%), desenvolvimento de sinais e sintomas típicos da doença como febre, tosse, dispnéia e fadiga (68,75%), linfopenia (68,75%), progressão para síndrome respiratória aguda grave (56,25%), necessidade de ventilação mecânica (50%) e admissão a intensivo (50%). Conclusões: Os pacientes em hemodiálise são mais suscetíveis à infecção por COVID-19 e, quando infectados pela SRA-CoV-2, estes pacientes têm resultados clínicos mais adversos, doenças mais graves, maior mortalidade e pior prognóstico do que a população em geral. As repercussões da COVID-19 em pacientes de hemodiálise revelam uma necessidade de cuidados preventivos de enfermagem em clínicas de hemodiálise.
Palavras-Chave: SARS-CoV-2; COVID-19; Diálise Renal; Insuficiência Renal Crônica; Enfermagem.
Introduction
COVID-19 is a highly contagious disease, whose cases range from mild to severe. It is considered a systemic disease that affects multiple organs and the kidneys are one of the most common organs affected by SARS-CoV-21. Specific groups of patients, such as those with chronic non-communicable diseases, are more likely to develop severe acute respiratory syndrome (SARS)1.
Patients with chronic kidney disease (CKD) are among the population considered at risk for severe COVID-19, especially those with associated comorbidities including diabetes mellitus and systemic arterial hypertension2. In 2017, the global estimated prevalence of CKD was 9.1%3. Hemodialysis stands out among the treatment modalities available for patients with CKD, being adopted by 92% of patients with this condition.
Patients with CKD are exposed to the virus more frequently than the general population, as they need to go out for hemodialysis sessions2. Given the impossibility of maintaining social isolation and abandoning treatment (essential for the maintenance of life), patients with CKD are more likely to become infected and develop severe SARS-CoV-2 infection4. In addition to the above, hemodialysis requires intensive care due to the possibility of clinical complications.
Since nurses are at the front line fighting the COVID-19 pandemic, they occupy a prominent position in the care of patients affected by this infection. These professionals also play an essential role in the hemodialysis service. With the advent of the COVID-19 pandemic, and due to the vulnerability of hemodialysis patients, nurses' responsibilities have become greater as it is necessary to coordinate efforts to prevent and control the transmission of the coronavirus5.
Issues related to signs, symptoms, and clinical outcomes prevalent in this population need to be elucidated, as few studies address the effects of COVID-19 in hemodialysis patients. Therefore, the following research question arose: What are the repercussions of COVID-19 in patients undergoing hemodialysis? This study's findings may be relevant to understanding the effects of COVID-19 infection in hemodialysis patients, facilitating the decision-making of nurses fighting this pandemic.
The aim of this systematic review was to identify the scientific evidence about the repercussions of COVID-19 in hemodialysis patients.
Materials and Methods
A systematic review of the literature was conducted. The review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines6. The review protocol was registered in PROSPERO. The research question for the systematic review was developed based on the PECOS framework7 (Table1). The research question was: What are the repercussions of COVID-19 in hemodialysis patients?
Table 1. Research question development process using the PECOS framework.
Element definition |
|
Description |
Population |
|
Patients undergoing hemodialysis treatment |
Exposure |
|
COVID-19 |
Comparator |
|
Not applicablea |
Outcome |
|
Repercussions of COVID-19 in hemodialysis patients |
Study design |
|
Observationalb and experimental research |
The inclusion criteria were primary studies, available online, published from 2019 to 2021, in any language, and studies addressing the repercussions or impacts of COVID-19 in hemodialysis patients. The literature search was carried out in February 2021 through the electronic databases: Cochrane Library, Web of Science, and Science Direct. In addition, PubMed and the Virtual Health Library were searched using direct access. The search strategies were determined using the MeSH and DeCS (Portuguese Health Sciences Descriptors) terms presented in Table2.
Table 2. Database search strategies.
Database |
|
PubMed |
|
Virtual Health Library |
|
Cochrane |
|
Web of Science |
|
Science Direct |
|
The eligibility of the articles took place in two stages. In the first stage, two independent reviewers evaluated the titles and abstracts and identified potentially eligible studies. In the second stage, the full texts were read to confirm eligibility. Any disagreement was resolved by consensus or by a third reviewer. Duplicates were identified and removed through the Mendeley Desktop platform version 1.19.4. Data related to findings reported in the present manuscript were saved as a dataset (Mendeley Data)8.
The methodological quality of the studies was assessed using the adapted Downs and Black checklist, which allows the assessment of the risk of bias in randomized and non-randomized studies9. In the present study, questions 4, 8, 12, 13, 14, 15, 19, 23, 24, and 27 were excluded because they refer to studies with a randomized clinical trial design, not retrieved in this research. Thus, 17 items from the original scale were used. Previous studies judged their articles according to the following categories: low methodological quality (=33.3%), moderate methodological quality (33.4–66.7%), and high methodological quality (=66.8%)10. Thus, we followed this same categorization in the present review.
The articles were assessed for quality according to criteria defined by the Oxford Center for Evidence-Based Medicine11. As we included studies with different methodological designs, meta-analysis was not performed, and the data synthesis was qualitative.
Results
Initially, the research enabled the inclusion of 163 studies, and of these, 22 duplicates were excluded. After the full-text screening, 125 articles were excluded for not meeting all the inclusion criteria. At the end of the selection process, 16 studies composed the final sample (Figure1).
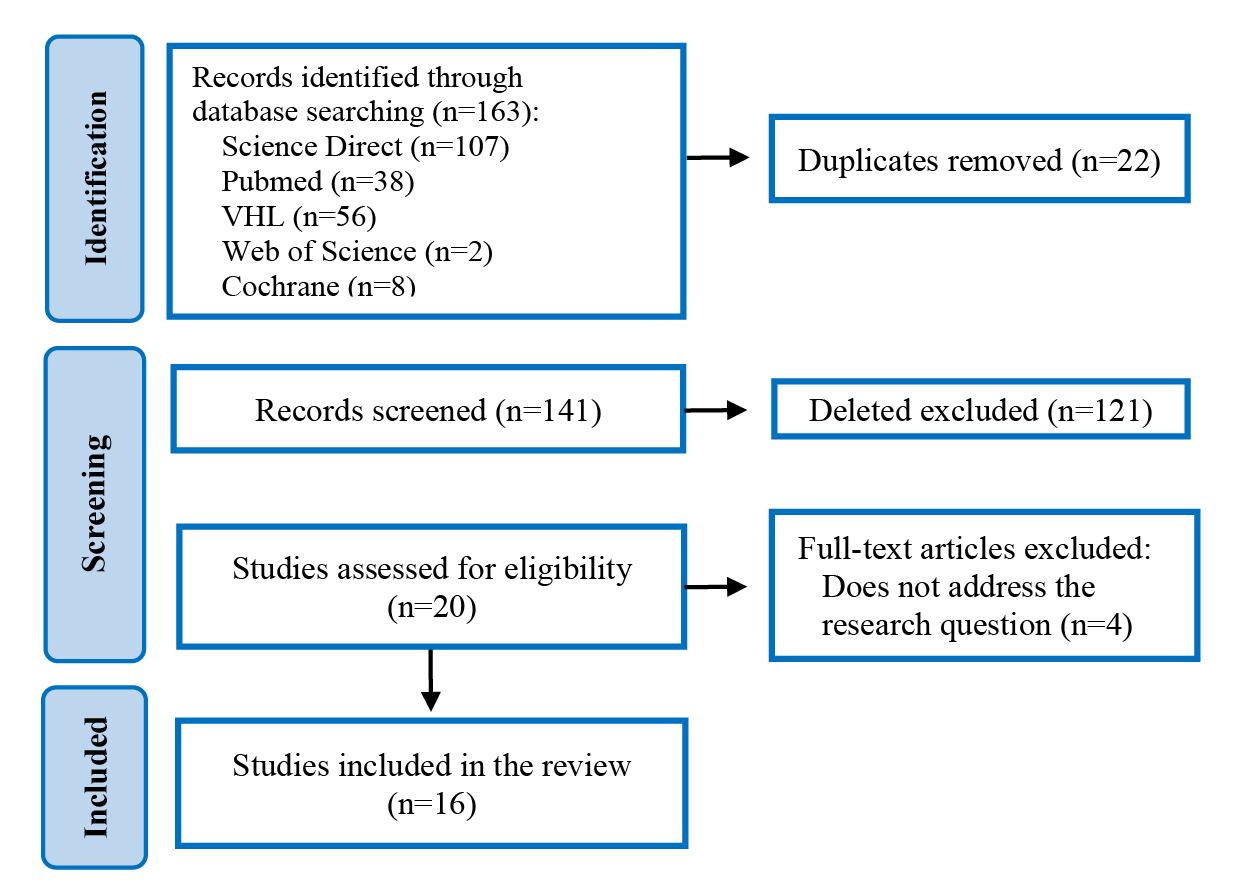
Figure 1: PRISMA Flowchart of the search strategy.
Of the 16 articles analyzed, 13 (81.25%) were cohort studies, two (12.5%) were case-control studies, and one was a cross-sectional study. As for the quality assessment, all articles had a percentage above 66.8% (high methodological quality). Regarding the level of evidence, studies classified as 2B (cohort studies) predominated (n=13; 81.25%). Table3 shows detailed information of the articles included in the final review sample.
Table 3. Synthesis of the articles included in the systematic review.
|
Author and year |
Location and sample |
Article title |
Design and Evidence level |
|
|
| A1 |
Ossareh et al./ 202012 |
Iran n=178 |
Role of Screening for COVID-19 in Hemodialysis Wards, Results of a Single Center Study. | Cohort Level 2B |
|
|
| A2 |
Zhang et al./ 202013 |
China n=31 |
Clinical characteristics of 31 hemodialysis patients with 2019 novel coronavirus: a retrospective study. | Cohort Level 2B |
|
|
| A3 |
Alberici et al./ 202014 |
Italy n=643 |
A report from the Brescia Renal COVID Task Force on the clinical characteristics and short-term outcome of hemodialysis patients with SARS-CoV-2 infection. | Cohort Level 2B |
|
|
| A4 |
Goicoechea et al./ 202015 |
Spain n=36 |
COVID-19: clinical course and outcomes of 36 hemodialysis patients in Spain. | Cohort Level 2B |
|
|
| A5 |
Wu et al./ 20205 |
China n=101 |
Clinical Features of Maintenance Hemodialysis Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. | Case-control Level 3B |
|
|
| A6 |
Sánchez-Pérez et al./ 202016 |
Valencia n=478 |
Results of a healthcare organization model for COVID-19 in hemodialysis in a tertiary hospital and its subsidized centres. | Cohort Level 2B |
72% |
|
| A7 |
Ebana et al./ 202117 |
Cameroon n=57 |
Epidemiologic and clinical profile, 90 days survival of incident end stage renal patient in haemodialysis during SARS-CoV2 pandemic: Experience of the General Hospital of Douala. |
Cohort Level 2B |
94% |
|
| A8 |
Savino et al./ 202018 |
United Kingdom n=2.385 |
Sociodemographic features and mortality of individuals on haemodialysis treatment who test positive for SARS-CoV-2: A UK Renal Registry data analysis. | Cohort Level 2B |
72% |
|
| A9 |
Albalate et al./ 202019 |
Madrid n=90 |
High prevalence of asymptomatic COVID-19 in hemodialysis. Daily learning during first month of COVID-19 pandemic. | Cross-sectional Level 4 |
67% |
|
| A10 |
Giaime et al./ 202020 |
France n=24 |
Hydroxychloroquine and azithromycin tolerance in haemodialysis patients during COVID-19 infection. | Cohort Level 2B |
94% |
|
| A11 |
Ozturk et al./ 202021 |
Turkey n=1.210 |
Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: a nationwide analysis from Turkey. | Case-control Level 3B |
94% |
|
| A12 |
Bell et al./ 202022 |
Scotland n=86 |
COVID-19 in patients with chronic kidney replacement therapy and kidney transplant recipients in Scotland: findings and experience from the Scottish renal registry. | Cohort Level 2B |
100% |
|
| A13 |
Cunha et al./ 202023 |
Spain n=48 |
The Spectrum of Clinical and Serological Features of COVID-19 in Urban Hemodialysis Patients. |
Cohort Level 2B |
78% |
|
| A14 |
Keller et al./ 202024 |
France n=123 |
Impact of first-wave Coronavirus disease 2019 infection in patients on haemodialysis in Alsace: the observational covidial study. | Cohort Level 2B |
78% |
|
| A15 |
Trivedi et al./ 202025 |
India n=37 |
Impact of COVID-19 on maintenance hemodialysis patients: The Indian scenario. | Cohort Level 2B |
67% |
|
| A16 |
Hendra et al./ 202126 |
United Kigndom n=148 |
Identifying prognostic risk factors for poor outcome following COVID19 disease among incentre haemodialysis patients: role of inflammation and frailty. | Cohort Level 2B |
89% |
The main results of the included studies show that laboratory abnormalities and poor clinical outcomes are common in hemodialysis patients with COVID-19. Table4 and Figure2 summarizes the impacts and repercussions of COVID-19 in hemodialysis patients.
Table 4. Impacts of COVID-19 in hemodialysis patients.
| Complications | Impact of COVID-19 in hemodialysis patients |
|
Frequency of studies |
||
| General |
Increased mortality rate Need for mechanical ventilation ICU admission Organ damage, cardiovascular complications, shock, and acute lung edema Decrease in duration and frequency of hemodialysis |
|
75% (n=12) 50% (n=8) 50% (n=8) 18.75% (n=3)
12.5% (n=2) |
||
| Respiratory |
|
|
68.75% (n=11) 56.25% (n=9) |
||
| Hematologic | Lymphopenia Albumin or glucose decrease Elevated D-dimer levels Elevated ferritin levels Elevated troponin T levels Elevated phosphorus levels |
|
68.75% (n=11) 25% (n=4) 25% (n=4) 18.75% (n=3) 18.75% (n=3) 12.5% (n=2) |
||
| Gastrointestinal | Gastrointestinal symptoms (diarrhea, nausea, or vomiting) Anorexia. |
|
31.25% (n=5) 12.5% (n=2) |
||
| Neurological | Uremic encephalopathy |
|
6.25% (n=1) |
It was observed that the most cited repercussions of COVID-19 in hemodialysis patients are related to general complications, such as high mortality (75%), respiratory complications and exacerbation of symptoms such as cough, dyspnea, fever and fatigue (68.75%), and progression to SARS (56.25%). Below is a graphical outline of the repercussions of COVID-19 on hemodialysis patients, classified according to their severity (Figure2)
Figure 2. Repercussions of COVID-19 in hemodialysis patients.

Discusión
In general terms, it was observed that the repercussions of the disease were similar across the studies, and they are related to the immunodeficiency status resulting from the kidney disease itself.
Studies indicate that hemodialysis patients are more likely to develop severe COVID-19 infection and SARS and that hemodialysis patients had more severe infection rates than the general population13. The uremic state that affects patients with CKD and the immunosuppression explain the high incidence of COVID-19 infection in these patients12,19.
The typical symptoms of COVID-19 presented by hemodialysis patients are the same as the general population and include fever, cough, dyspnea, and fatigue. However, research has pointed out that hemodialysis patients infected with COVID-19 may not have a fever, as the incidence of hypothermia in this population is frequent27. Previous testing for COVID-19 through an individualized approach in hemodialysis patients can be a relevant strategy to optimize diagnostic accuracy and adequate control of virus transmissibility among patients, healthcare staff, and other contacts.
Given the complications caused by COVID-19, many patients on hemodialysis were admitted to intensive care units and needed mechanical ventilation. Another respiratory complication evidenced is acute lung edema17. In addition to SARS, a case-control study concluded that hemodialysis patients were more likely to develop shock and acute cardiac arrest5.
In this context of hospitalization and admission of these patients in intensive care units, nursing care in the hospital environment must be provided efficiently and integrated to the multidisciplinary team. A series of nursing actions must be carried out to promote the patients' safety, such as infection control measures, oral hygiene, aspiration of secretions, and vital signs monitoring. It is essential that the assistance of health professionals, especially nurses, in whatever environment the patient is in, is provided holistically and systematically to ensure correct and efficient interventions that improve patient outcomes.
Concerning gastrointestinal manifestations, studies show that diarrhea, nausea, vomiting, and respiratory symptoms were more intense and frequent in hemodialysis patients with COVID-1928. In this scenario, the role of nurses working in outpatient clinics and hemodialysis clinics should be directed towards carrying out a holistic assessment of the patient, seeking to identify the phenomena resulting from hemodialysis therapy or COVID-19.
Among hematologic complications, several authors warn that lymphopenia is a prevalent laboratory finding in COVID-19 patients, being significantly more frequent in CKD patients on hemodialysis. A study comparing blood test results before and after COVID-19 infection showed that 51.6% of patients had a significant decrease in lymphocyte count13,15,26. Lymphopenia should be considered part of the diagnosis and a risk marker, especially in hemodialysis patients.
Another significant blood abnormality found was increased D-dimer, a marker of vascular damage. This abnormality was detected in 31 hemodialysis patients with COVID-19 in Wuhan, China, where 96.8% had increased D-dimer13. D-dimer is a marker that is elevated in hemodialysis patients. However, this increase was approximately three times greater than the normal values (68–494 µg) in hemodialysis patients with COVID-1923.
Decreased albumin and glucose levels were laboratory findings described in many studies13,15,21,26,. Existing evidence suggests that the inflammatory state, evidenced by elevated C-reactive protein levels, can suppress albumin synthesis in hemodialysis patients29. In this context, care nurses and nephrologists need to recognize early predictive signs of complications presented by chronic renal patients to provide quick, timely, and adequate care.
Some authors also describe that hemodialysis patients with COVID-19 had higher values of phosphorus than the general population5,13,. This is due to the excessive intake of foods rich in phosphorus and the low efficiency in removing phosphorus from plasma by the dialysis method. The role of nurses in educating patients on eating a balanced diet is important and enables the establishment of effective communication with patients and family members, facilitating treatment adherence and, consequently, a better quality of life.
An analysis in Peru compared patients hospitalized with COVID-19 at various stages of kidney disease and found that ferritin levels were significantly higher in those on hemodialysis23. For all this, ferritin can help screen COVID-19 in asymptomatic or non-symptomatic hemodialysis patients.
Researchers conducted a cohort study with hemodialysis patients and identified that troponin T levels were high in those with COVID-1920. Even without the association with cardiac lesions, high troponin levels indicate a worse prognosis26. In this context, when evaluating a patient with CKD, nurses should be aware of increased values of basal cardiac troponin T or I.
A study found that of 24 patients with COVID-19, 83.4% developed uremic encephalopathy17. As the nursing team is responsible for providing direct and indirect care to hemodialysis patients, it is up to these professionals to identify complications and initially assess the patients' clinical status to establish appropriate multidisciplinary conduct.
Although risk factors for COVID-19 are similar to the general population, patients on hemodialysis have a higher mortality rate. In an observational study in Spain, the authors found that hemodialysis patients with COVID-19 who died had lymphopenia, increased C-reactive protein and lactate dehydrogenase, and a longer time on hemodialysis treatment15. Given the above, it is essential to identify early risk factors and provide timely treatment for critical cases to reduce mortality and hospitalization in this highly vulnerable group.
In addition to the clinical effects, the repercussions of COVID-19 also influenced the dialysis treatment of patients on chronic dialysis regimens. Surveys show that a third of patients missed regular dialysis sessions13,25. In this sense, such treatment must be maintained during the pandemic, which involves care and procedures adopted by patients, health professionals, dialysis center managers, and health authorities.
As professionals who work on the front line in hospital, outpatient and clinical services, nurses have an essential role in the care of critically ill patients, as they carry out the planning of actions and the execution of work processes essential to quality patient care. The nursing team is a reference in the hemodialysis unit, providing direct care to patients who need this therapeutic modality to survive.
It is necessary to constantly update general nurses and specialists regarding the specifics of chronic renal patients undergoing renal replacement therapy. It is also recommended that the dialysis team always be aware of the signs and symptoms of COVID-19, in addition to managing transmission control. Although the pandemic scenario remains, it is important to maintain this treatment, considering the risks and benefits highlighted and discussed in the present study.
Among the study's limitations, it was observed that some studies were based on experiences developed in some institutions, which may differ from the reality of other locations. In addition, the small sample size of some studies is a limitation. In this sense, the results of this review highlighted the need for cross-sectional and cohort studies with larger sample sizes on hemodialysis patients with COVID-19 to understand better the repercussions of COVID-19 in this population.
It is believed that the information from this study may help health professionals in identifying potential risks to renal patients affected by SARS-CoV-2, in addition to facilitating the recognition of clinical priorities and potential supporting treatment, especially in those with a high risk of death.
Conclusión
People with CKD affected by SARS-CoV-2 have a worse prognosis and a high mortality rate. The major repercussions of COVID-19 in patients with CKD undergoing hemodialysis are general, such as the need for ICU admission, mechanical ventilation, and high mortality rate. In addition, the damage of target organs such as the heart, lungs, and shock has been described. The main complications found through the review divided by bodily systems are SARS (respiratory), uremic encephalopathy (neurological), nausea, vomiting, and anorexia (gastrointestinal), and blood abnormalities. Therefore, hemodialysis patients are more susceptible to severe COVID-19, especially those with associated comorbidities.
Conflicts of interest: the authors declare no conflicts of interest.
References