Rev Cuid. 2024; 15(3): e3558
Abstract
Introduction: The global prevalence of childhood obesity is a public health challenge. Early intervention, including during pregnancy, is essential to prevent this health problem. Objective: Identify and characterize interventions during the first 1000 days of life that effectively prevent overweight and obesity. Materials and Methods: A scoping review was carried out following the methodology proposed by Arksey and O'Malley. SCOPUS, EBSCOHost and PubMed databases were searched to select relevant articles. The analysis focused on articles published between January 2012 and December 2022. Results: Fourteen articles with 10 interventions were included. These interventions were implemented in high-income countries and in racial and ethnic groups. Three interventions, involving 1013 women and their children, reported significant effects on preventing overweight and obesity at 18 and 24 months of the child's life. Discussion: The interventions were characterized as multi-component, educational and based on theories of behavior change, parenting and sensory feeding. They addressed risk factors such as breastfeeding, complementary feeding, physical activity and sleep. There is an increasing use of digital technology in their delivery. Conclusion: Promising results have been found for the prevention of obesity in the early years of life; therefore, implementation of interventions in low- and middle-income countries is of paramount importance.
Keywords: Childhood Obesity; Overweight; Infant; Prevention.
Resumen
Introducción: La prevalencia mundial de la obesidad infantil plantea un desafío para la salud pública. Para prevenir este problema de salud, es crucial intervenir tempranamente, incluso durante el embarazo. Objetivo: Identificar y caracterizar intervenciones realizadas durante los primeros 1000 días de vida que eviten de manera efectiva el sobrepeso y la obesidad. Materiales y Métodos: Se realizó una revisión de alcance siguiendo la metodología propuesta por Arksey y O'Malley. Se realizaron búsquedas en las bases de datos SCOPUS, EBSCOHost y PubMed para seleccionar artículos relevantes. El análisis se centró en artículos publicados entre enero de 2012 y diciembre de 2022. Resultados: Se incluyeron 14 artículos que integraban 10 intervenciones. Estas fueron implementadas en países de altos ingresos y con grupos raciales/étnicos. Tres intervenciones, conformadas por 1013 mujeres y sus hijos, reportaron efectos significativos en la prevención de sobrepeso y obesidad a los 18 meses y 24 meses de edad del niño. Discusión: Las intervenciones se caracterizaron por ser multicomponentes, educativas, basadas en teorías de cambio de comportamiento, crianza de los hijos y alimentación perceptiva. Abordaron factores de riesgo como la lactancia materna, alimentación complementaria, actividad física y el sueño. Existe una creciente incorporación de tecnología digital en su implementación. Conclusión: Se han observado resultados prometedores para la prevención de la obesidad en los primeros años de vida. Implementar intervenciones en países de bajos y medianos ingresos resulta primordial.
Palabras Clave: Obesidad Infantil; Sobrepeso; Lactante; Prevención.
Resumo
Introdução: A prevalência global da obesidade infantil representa um desafio para a saúde pública. Para prevenir este problema de saúde é fundamental intervir precocemente, mesmo durante a gravidez. Objetivo: Identificar e caracterizar intervenções realizadas durante os primeiros 1000 dias de vida que previnam eficazmente o excesso de peso e a obesidade. Materiais e Métodos: Foi realizada uma revisão de escopo seguindo a metodologia proposta por Arksey e O'Malley. As bases de dados SCOPUS, EBSCOHost e PubMed foram pesquisadas para selecionar artigos relevantes. A análise centrou-se em artigos publicados entre janeiro de 2012 e dezembro de 2022. Resultados: Foram incluídos 14 artigos que integraram 10 intervenções. Estas foram implementadas em países de rendimento elevado e com grupos raciais/étnicos. Três intervenções, compostas por 1.013 mulheres e seus filhos, relataram efeitos significativos na prevenção do sobrepeso e da obesidade aos 18 meses e aos 24 meses de idade da criança. Discussão: As intervenções caracterizaram-se como multicomponentes, educativas, baseadas em teorias de mudança de comportamento, parentalidade e alimentação responsiva. Abordaram fatores de risco como amamentação, alimentação complementar, atividade física e sono. Há uma crescente incorporação da tecnologia digital na sua implementação. Conclusão: Resultados promissores foram observados para a prevenção da obesidade nos primeiros anos de vida. A implementação de intervenções em países de baixo e médio rendimento é essencial.
Palavras-Chave: Obesidade Infantil; Sobrepeso; Lactente; Prevenção.
Introduction
Over the past four decades, the global prevalence of childhood obesity has increased exponentially1, with 37 million children under the age of five being overweight or obese2. Being overweight or obese in the early years of life has been shown to increase the risk of developing a number of early diseases such as asthma, coronary heart disease, type 2 diabetes mellitus, osteoarthritis, some cancers and others3,4, and is responsible for 2.6 million deaths each year5. Preventing childhood obesity is therefore a priority6.
Early life is a critical period for the development of obesity. International child health organizations have developed guidelines and recommendations to prevent, control and reduce obesity during the first 1000 days7 - a crucial period of human development from conception to 2 years of age8. These recommendations aim to implement evidence-based interventions that comprehensively address key modifiable risk factors during the prenatal and postnatal stages to prevent childhood obesity9,10. It is, therefore, important to identify the types of interventions that have been implemented to prevent childhood obesity in the first 1000 days and whether they have evidence of effectiveness.
Previous systematic reviews have assessed interventions in these stages and found promising results; however, the prenatal or postnatal stages have been considered indistinctly11,12, so this review sought to assess only those interventions that considered both stages of development, as the evidence mentions the importance of considering the first 1000 days in a comprehensive way9. Therefore, the aim of this scoping review was to identify and characterize the interventions implemented in the first 1000 days (considering the prenatal and postnatal period together) for the prevention of overweight and obesity. The information gathered can serve as a guide for health care providers and researchers looking for opportunities to implement interventions aimed at preventing childhood obesity.
Materials and Methods
This a registered scoping review13,14, which used the 5 stages of Arksey and O'Malley's methodological framework15.
Research question identification
1) What international evidence exists on interventions that address the first 1000 days of life with the objective of preventing overweight and obesity in children under two years of age?
2) What are the characteristics of interventions that have been effective in preventing overweight and obesity in children under two years of age at the international level?
Relevant studies
In January 2023, a systematized search was conducted in the SCOPUS, EBSCOHost and PubMed databases, focused on the pre-established inclusion criteria and using the Medical Subject Headings (MeSH) vocabulary descriptors of the U.S. National Library of Medicine MeSH that included the words: infancy, infants, first 1000 days, preventive measures, prevention, control, intervention, overweight, obesity, body weight, pediatric obesity, randomized controlled trial, clinical trial randomized, systematic review.
Study selection
Criteria: Systematic reviews of randomized clinical trials and/or articles documenting a single randomized clinical trial; published between 1 January 2012 and 31 December 2022; interventions should consider the first 1000 days and focus on obesity prevention in children aged 0-2 years; with weight or BMI z-score by age as the primary outcome to homogenize and contrast studies; no language restriction. Non-systematic literature reviews, protocols, grey literature and pre-prints were excluded.
Charting the data
The PRISMA-ScR extension framework was used to extract the information. The information was recorded independently by two of the authors using a form.
Comparing, summarizing and communicating the results
The interventions were identified and summarized according to the patterns found in the extracted information15. The database was stored in Mendeley Data16.
Ethical aspects
The review studies do not require ethics committee approval, but scientific rigor was essential in their realization.
Results
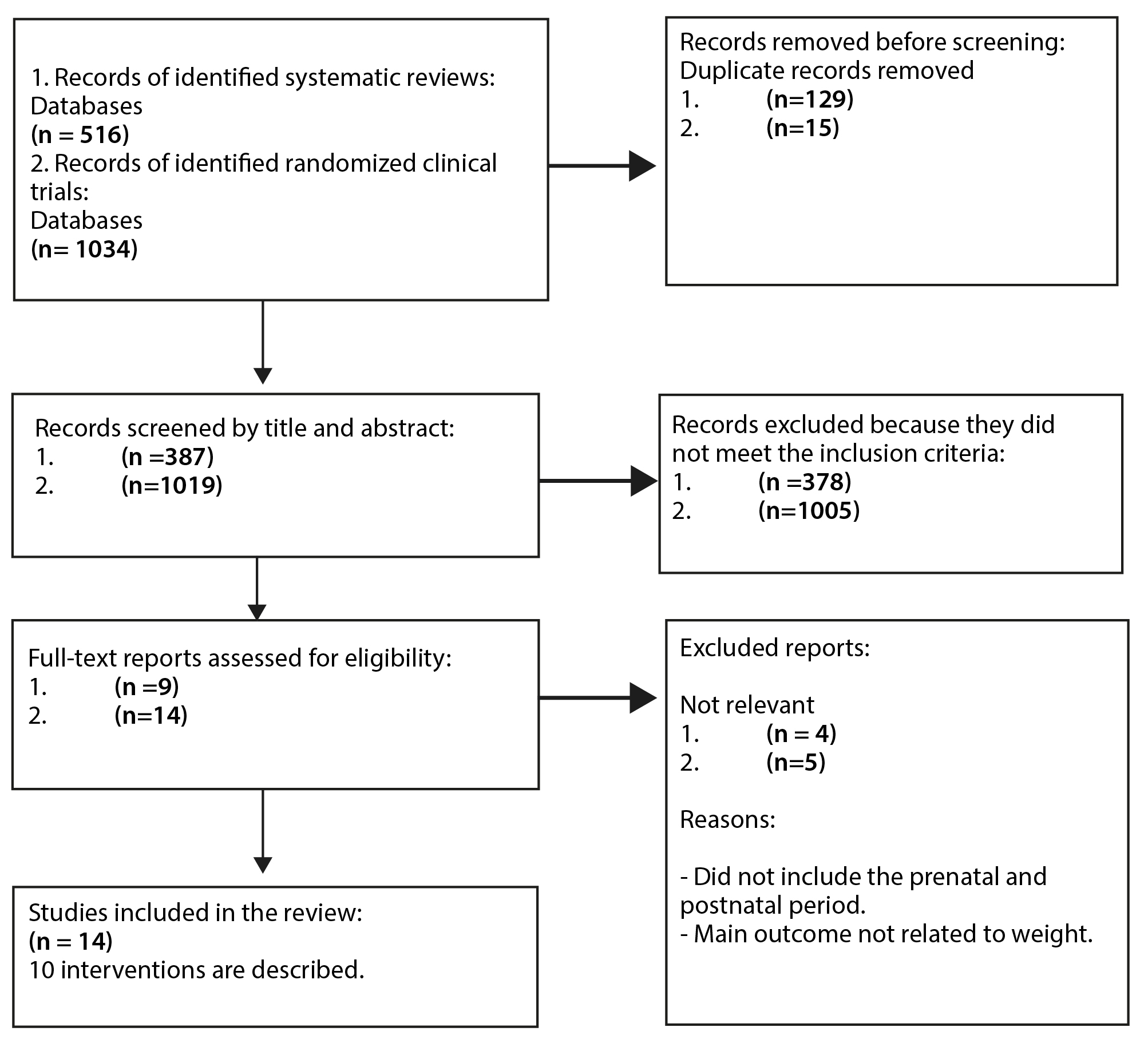
For interventions reported in systematic reviews, a total of 387 references were identified after removing duplicates; 378 were excluded based on title and abstract, leaving a total of 9 articles to be assessed in full text. The search was supplemented with a strategy to identify randomized clinical trials of individual interventions, of which 5 were excluded because they did not meet the criteria, and the remaining 9 trials were considered eligible. The total number of articles included in both searches was 14, comprising 10 interventions17-30. See Figure 1.
In order to answer the research questions, the corresponding articles were reviewed, and the results were categorized along three main dimensions: characteristics of the study population, characteristics of the intervention design, general characteristics and outcomes of effective interventions.
Study population characteristics
All interventions were carried out in high-income countries, none in middle- or low-income countries. Participants were women aged over 18 years from low socioeconomic backgrounds. Four of them belonged to the Latino subcultural group, one to the African American group, and the rest were not specified (n=5). Half of the interventions (n=5) started when the mother was in the third quarter of pregnancy, and the rest in the second and third quarters (n=5). See Table 1.
Table 1. General characteristics of the study population, 2012-2022
X
Table 1. General characteristics of the study population, 2012-2022
| Author/Year |
Country of Residence |
Mother's Age |
Socioeconomic Status |
Subcultural Group |
Pregnancy Stage |
Reifsnider et al., 201817; McCormick et al., 202018 |
United States |
18 to 40 years old |
Low |
Latinas |
Third quarter |
Gross et al., 201619; Messito et al., 202020 |
United States |
Over 18 years old |
Low |
Latinas/Hispanics |
Third quarter |
| Ordway et al., 201821 |
United States |
14 to 25 years old |
Low |
Different ethnic communities/Hispanics |
Third quarter |
| Parat et al., 201822 |
France |
18 years and older |
Low |
Not specified |
Equal to or less than 21 weeks of gestation |
Fangupo 201523; Taylor et al., 201724 Taylor et al., 201825 |
New Zealand |
16 years and older |
Not specified |
Not specified |
Before 34 weeks of gestation |
| Fiks et al., 201726 |
United States |
18 years and older |
Low |
Not specified |
Third quarter |
| Thomson et al., 201827 |
United States |
18 years and older |
Low |
Not specified |
Minimum 19 weeks of gestation |
| Wasser et al., 202028 |
United States |
18 to 39 years old |
Low |
Non-Hispanic African Americans |
28 weeks of gestation |
| Wen et al., 201229; 201530 |
Australia |
Over 16 years old |
Low |
Not specified |
Between 24 and 34 weeks of gestation |
Design characteristics of the interventions
Seven interventions used behavior change theory in their design, with social cognitive theory being the most commonly used. All interventions were face-to-face and delivered mainly by nurses and dietitians. The duration of the interventions ranged from 2 to 3 years.
Although all the interventions started in the prenatal period, only two of them addressed maternal factors, such as gestational weight gain. The others developed educational programs that focused on postnatal factors, such as infant nutrition.
Integration of physical activity and sleep was less common. Finally, the Starting Early Program (StEP)20, Minding the Baby21, and Healthy Beginnings29,30 interventions were found to have statistically significant outcomes related to infant weight. See Table 2.
Table 2. Design characteristics of the total number of interventions identified for the period 2012-2022
X
Table 2. Design characteristics of the total number of interventions identified for the period 2012-2022
| Author/Year |
Theoretical Framework |
Delivery |
Duration |
Environment and Number of Sessions |
Attention to Intervention Group |
Attention to Control Group |
Primary Outcomes |
Findings |
Reifsnider et al., 201817 McCormick et al., 202018 |
Not specified |
Face-to-face. |
2 years |
Home.9 sessions: 36 weeks gestation, 2 weeks of age, 2, 4, 6, 9, 12, 18 and 24 months. |
Child growth, breastfeeding, nutrition, physical activity and sleep. |
Visits for measuring child growth and development. |
Weight-for-length z-score of infants |
Parents' education did not reduce childhood overweight. |
Gross et al., 201619 Messito et al., 202020 |
Social Cognitive Theory |
Face-to-face. Certified dietitians as lactation counselors. |
3 years |
Primary care clinics. 17 sessions: 4 individual (third quarter) and 13 in groups (postpartum) at 1, 2, 4, 6, 9, 12, 15, 18, 21, 24, 27, 30 and 33 months. |
Nutrition, breastfeeding and parenting. |
The usual care. |
Weight-for-height z-score and weight-for-age z-score, prevalence of obesity and excessive weight gain from birth to 2 years of age. |
Mean weight-for-age z-scores and growth trajectories were lower in the intervention group up to 2 years. |
| Ordway et al., 201821 |
Socio-Ecological Model |
Face-to-face. Social Worker with Master's Degree and Pediatric Nurse. |
2 years |
Home or place of convenience for the mother.Approximately 78 sessions (1 visit per week for 1 year, then fortnightly for 1 year). |
Parent-child attachment, maternal reflective functioning and positive parenting behaviors. |
The usual care. |
Prevalence of overweight or obesity in children at 2 years of age. |
More children in the intervention group had a healthy body mass index at 2 years of age. |
| Parat et al., 201822 |
Not specified |
Face-to-face. Physician, dietician, midwife. |
27 weeks |
Hospital. 6 sessions: 2 individual prenatal sessions (26 and 30 weeks of gestation and 4 group sessions (21, 28, 35 weeks of gestation, 2 months Postpartum). |
Infant and maternal feeding |
The usual care. |
Infant weight gain from birth to 2 years of age. |
Excessive weight gain during pregnancy was not significantly changed. Overweight in mothers and children 2 years after delivery was not prevented. |
Fangupo 201523 Taylor 201724, 201825 |
Responsive Parenting |
Face-to-face. Parents as Teachers (PAT): lactation consultant, trained researchers (nurses, dietitians, nutrition graduates). Sleep: nurse researcher; COMBO: includes both of the above. |
18 months |
Home and group. 8 sessions: 5 pre-delivery visits (3 face-to-face and 2 by telephone), postpartum 3 additional face-to-face contacts at 3, 9 and 18 months. |
Food, activity and breastfeeding (FAB): Healthy eating, breastfeeding, physical activity. |
Sleep or a combination (FAB plus Sleep) |
Child's body mass index. |
Food, activity and breastfeeding (FAB) had an unexpected long-term adverse effect (weight gain). A protective effect for obesity in those who received the 'sleep intervention'. |
| Fiks et al., 201726 |
Social Learning Theory |
Face to face. Facebook. Psychologist. |
11 months |
Hospital/Facebook. 2 face-to-face and follow-up via Facebook. |
Infant feeding practices, sleep, positive parenting, maternal well-being. |
Reminders for infant primary care visit |
Weight-for-height z-score. |
No significant differences in anthropometric parameters were found. |
| Thomson et al., 201827 |
Social Cognitive Theory and Transtheoretical Model of Behavioral Change |
Face-to-face. University educated women and trained in Parents as Teachers (PAT) curriculum. |
18 months |
Home. 17 sessions: 5 prenatal visits, 12 postnatal visits per month on average. |
Parents as Teachers plus weight control, gestational and postnatal physical activity, breastfeeding, complementary feeding, tummy time and sedentary lifestyles |
Parents as Teachers (PAT) training, parents' knowledge of child development, improving parenting practices, providing early detection of developmental delays. |
Gestational weight gain. Weight status.Weight-for-height z-score, Weight-for-age z-score, Body Mass Index. |
It was not effective in improving maternal weight and infant growth outcomes. |
| Wasser et al., 202028 |
Not specified |
Face-to-face. Peer educator. |
15 months |
Home. 6 sessions: 1 during pregnancy and at 3, 6, 9, 12 and 15 months after childbirth. |
Mindful and responsive feeding practices. |
Child safety guidance. |
Weight-for-height z-score, Weight-for-age z-score, Body Mass Index. |
It did not produce significant differences in infant growth. |
| Wen et al., 201229; 201530 |
Social Learning Theory and the Health Belief Model |
Face-to-face. Community nurse. |
2 years |
Home. 8 sessions: (1 prenatal and at 1, 3, 5, 9, 12, 18 and 24 months) |
Breastfeeding, complementary feeding, tummy time, active play, family nutrition, physical activity and sleep. |
The usual care. |
Body Mass Index. |
It was effective in reducing the average Body Mass Index of two-year-olds. |
General characteristics and outcomes of effective interventions
Finally, as this is a scoping review, we did not carry out a comprehensive analysis of outcomes31; however, we found that effective interventions were delivered to pregnant women from the third quarter onwards. According to the components, these interventions were based on the major risk factors for childhood obesity, supported by cognitive-behavioral theories. Delivery was face-to-face, mainly by nurses, and the impact of the intervention was influential in maintaining or improving nutritional status. This is described in Table 3.
Table 3. General characteristics and outcomes of effective interventions to prevent overweight and obesity in the first 1000 days of life
X
Table 3. General characteristics and outcomes of effective interventions to prevent overweight and obesity in the first 1000 days of life
| Author/Year |
Intervention Name |
Delivered by/Components |
Environment and Sessions |
Outcomes of Intervention vs. Control |
| Messito et al., 202020 |
Starting Early Program |
Registered dietitians as lactation consultants. Social Cognitive Theory, Nutrition, breastfeeding and parenting. |
Primary care clinics. 17 sessions, 4 individual sessions in the third quarter and 13 group sessions from 1 to 33 months of age. |
The infants in the intervention group had a lower weight-for-age z-score at 18 months (0.49 vs. control 0.73, p = 0.04) and at 2 years (0.56 vs. 0.81, p = 0.03). |
| Ordway et al., 201821 |
Minding the Baby |
Social workers and pediatric nurses.Socio-ecological model. Parent-child attachment, maternal reflective functioning and positive parenting behaviors. |
Home visits. Weekly pediatric sessions from the third quarter of pregnancy until the child's first birthday, and then every two weeks until the child's second birthday. |
The rate of obesity was significantly higher (p = 0.01) in the control group (19.70%) compared to the intervention group (3.30%) at 2 years (odds ratio = 0.32, 95% CI [0.13-0.78] p = 0.01). |
| Wen et al., 2012; 201529,30 |
Healthy Beginnings |
Community nurses. Social Learning Theory and Health Beliefs. Breastfeeding, complementary feeding, tummy time, active play, family nutrition, physical activity and sleep. |
Home visits. One visit in the prenatal period and 7 visits at 1-24 months of age. |
The mean BMI was significantly lower in the intervention group (16.53) than in the control group (16.82), with a difference of 0.29 (95% CI [-0.55-0.02] p = 0.04). |
Discussion
The aim of this study was to identify and characterize interventions delivered during the first 1000 days of life for the prevention of childhood obesity. We identified 10 interventions reported in 14 articles between 2012 and 2022.
We found that the development and implementation of interventions are concentrated in high-income countries, in line with other systematic reviews11,12,32, and that while in the past overweight was almost exclusively a problem of high-income countries, prevalence patterns have now changed, with low- and middle-income countries accounting for three-quarters of childhood overweight worldwide2,33. Policies focusing on the prevention of childhood obesity in the first 1000 days have recently been implemented in Latin America34 and publications from this region with positive results are expected soon.
More than half of the interventions included racial/ethnic subgroups in their study populations, such as Latinos and African Americans, who are considered to be groups with a high prevalence of risk factors for childhood obesity35,36; however, they did not include cultural or environmental aspects beyond the vulnerability or ethnicity of the population, which is seen as an area of opportunity. This highlights the need for future interventions to consider the socioeconomic status, environment and culture in which children and families live, as these variables may influence weight-related behaviors, as do dietary practices and physical activity37,38.
Regarding the start of implementation, most interventions were initiated in the third quarter of pregnancy; however, evidence suggests that ideally they should be initiated before conception, but if this is not possible, they should be initiated from the first quarter of pregnancy and continued until the child is two years old39. As previously mentioned, it was found that none of the interventions included preconception care, but they did include follow-up for two years or more, which aligns with the scientific evidence reported in previous systematic reviews11,12,40. Preventive interventions delivered at these stages may prepare the mother-to-be to reduce risk factors for childhood obesity, and there is, therefore, a need to continue to research this period8,9,11,38.
This scoping review found three interventions with statistically significant results: StEP20, Minding the Baby21 and Healthy Beginnings29. Key features of these interventions were that they were multi-component and targeted the main risk factors for obesity in early childhood; they also used theoretical models that focus on how perceptions, beliefs and thoughts influence behavior. This allows for a coherent, evidence-based structure that facilitates the understanding of health determinants, the prediction and evaluation of outcomes, and the reproducibility and generalizability of interventions6,9,41.
The delivery method for these three interventions was face-to-face home visits, with a minimum follow-up of 2 years. Evidence suggests that, beyond the provision of information, this individualized face-to-face support builds a relationship of trust between the facilitator and the mother, promoting favorable outcomes in terms of improvements in developmental indicators, infant feeding practices and parenting, all in disadvantaged families42,43.
Likewise, it was seen that the use of technology was incorporated into the interventions, the most common being telephone calls, text messages and computer use. The use of technological resources to promote health is an opportunity to bring educational strategies to the population44. In recent years, the number of people using these tools on a daily basis has increased, providing an opportunity for educators and researchers to reduce the cost of implementing obesity prevention interventions, thus reducing the gap in access to health services45,46.
Cultural adaptations are considered necessary to improve identified outcomes47, and the use of technology and interventions that take into account multifactorial aspects such as culture, dietary practices and physical activity has significant effects on participants' weight32,48.
Limitations include the fact that, by its nature, this scoping review did not include a quality assessment of the reviewed studies or an in-depth review of the statistical results, which may limit the generalizability of the findings. Strengths include that the design allowed for a systematic synthesis of research characteristics and findings, which could contribute to health professionals' decision-making in preventing of childhood obesity.
Conclusion
It is encouraging that from the ten selected interventions, three were found to be effective in preventing childhood overweight and obesity in the first 1000 days of life. The characteristics summarized in terms of study population, intervention design and outcomes of effective interventions provide evidence that can be used to determine whether these interventions will work in other contexts, such as low- and middle-income countries and in groups vulnerable to developing childhood obesity.
In addition, the use of cultural adaptation processes could be a useful strategy to reduce development and implementation time and optimize resources. Ensuring that interventions cover all of the above aspects will result in better prevention of childhood obesity.
Conflict of Interest: The authors stated that there is no conflict of interest.
Funding: This research was not funded.
References
X
Referencias
Horesh A, Tsur AM, Bardugo A, Twig G. Adolescent and Childhood Obesity and Excess Morbidity and Mortality in Young Adulthood—a Systematic Review. Curr Obes Rep. 2021;10:301–10. https://doi.org/10.1007/s13679-021-00439-9
X
Referencias
Deal BJ, Huffman MD, Binns H, Stone NJ. Perspective: Childhood Obesity Requires New Strategies for Prevention. Advances in Nutrition. 2020;11(5):1071–8. https://doi.org/10.1093/ADVANCES/NMAA040
X
Referencias
Larqué E, Labayen I, Flodmark CE, Lissau I, Czernin S, Moreno LA, et al. From conception to infancy — early risk factors for childhood obesity. Nat Rev Endocrinol. 2019;15:456–78. https://doi.org/10.1038/S41574-019-0219-1
X
Referencias
Schwarzenberg SJ, Georgieff MK, Daniels S, Corkins M, Golden NH, Kim JH et al. Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics. 2018;141(2):e20173716. https://doi.org/10.1542/peds.2017-3716
X
Referencias
Pietrobelli A, Agosti M, MeNu Group. Nutrition in the First 1000 Days: Ten Practices to Minimize Obesity Emerging from Published Science. Int J Environ Res Public Health. 2017;14(12):1491. https://doi.org/10.3390/IJERPH14121491
X
Referencias
Karacabeyli D, Allender S, Pinkney S, Amed S. Evaluation of complex community-based childhood obesity prevention interventions. Obes Rev. 2018;19(8):1080–92. https://doi.org/10.1111/OBR.12689
X
Referencias
Hennessy M, Heary C, Laws R, van Rhoon L, Toomey E, Wolstenholme H, et al. The effectiveness of health professional-delivered interventions during the first 1000 days to prevent overweight/obesity in children: A systematic review. Obes Rev. 2019;20(12):1691–707.https://doi.org/10.1111/OBR.12924
X
Referencias
Blake-Lamb TL, Locks LM, Perkins ME, Woo Baidal JA, Cheng ER, Taveras EM. Interventions for Childhood Obesity in the First 1,000 Days A Systematic Review. Am J Prev Med. 2016;50(6):780–9. https://doi.org/10.1016/J.AMEPRE.2015.11.010
X
Referencias
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73. https://doi.org/10.7326/M18-0850
X
Referencias
Zepeda PA, Cárdenas VM, Sifuentes DC. Interventions for early prevention of childhood obesity during the first 1000 days: A scoping review protocol 2023. https://doi.org/10.17605/OSF.IO/5BAMK
X
Referencias
Zepeda PA, Cárdenas VM, Sifuentes DC, Guevara MC. Intervenciones para prevenir la obesidad en los primeros 1000 días: Scoping Review - Mendeley Data V1. https://doi.org/10.17632/zvk4wby72y.1
X
Referencias
Reifsnider E, McCormick DP, Cullen KW, Todd M, Moramarco MW, Gallagher MR, et al. Randomized Controlled Trial to Prevent Infant Overweight in a High-Risk Population. Acad Pediatr. 2018;18(3):324–33. https://doi.org/10.1016/J.ACAP.2017.12.007
X
Referencias
Gross RS, Mendelsohn AL, Gross MB, Scheinmann R, Messito MJ. Randomized Controlled Trial of a Primary Care-Based Child Obesity Prevention Intervention on Infant Feeding Practices. J Pediatr. 2016;174:171-177. https://doi.org/10.1016/J.JPEDS.2016.03.060
X
Referencias
Messito MJ, Mendelsohn AL, Katzow MW, Scott MA, Vandyousefi S, Gross RS. Prenatal and Pediatric Primary Care-Based Child Obesity Prevention Program: A Randomized Trial. Pediatrics. 2020;146(4):e20200709. https://doi.org/10.1542/peds.2020-0709
X
Referencias
Ordway MR, Sadler LS, Holland ML, Slade A, Close N, Mayes LC. A Home Visiting Parenting Program and Child Obesity: A Randomized Trial. Pediatrics. 2018;141(2). https://doi.org/10.1542/PEDS.2017-1076
X
Referencias
Parat S, Nègre V, Baptiste A, Valensi P, Bertrand AM, Chollet C, et al. Prenatal education of overweight or obese pregnant women to prevent childhood overweight (the ETOIG study): an open-label, randomized controlled trial. Int J Obes (Lond). 2019;43:362–73.https://doi.org/10.1038/S41366-018-0205-Z
X
Referencias
Fangupo LJ, Heath ALM, Williams SM, Somerville MR, Lawrence JA, Gray AR, et al. Impact of an early-life intervention on the nutrition behaviors of 2-y-old children: a randomized controlled trial. Am J Clin Nutr. 2015;102(3):704–12. https://doi.org/10.3945/AJCN.115.111823
X
Referencias
Taylor RW, Williams SM, Fangupo LJ, Wheeler BJ, Taylor BJ, Daniels L, et al. Effect of a Baby-Led Approach to Complementary Feeding on Infant Growth and Overweight: A Randomized Clinical Trial. JAMA Pediatr. 2017;171(9):838-846. https://doi.org/10.1001/JAMAPEDIATRICS.2017.1284
X
Referencias
Taylor RW, Gray AR, Heath ALM, Galland BC, Lawrence J, Sayers R, et al. Sleep, nutrition, and physical activity interventions to prevent obesity in infancy: follow-up of the Prevention of Overweight in Infancy (POI) randomized controlled trial at ages 3.5 and 5 y. Am J Clin Nutr. 2018;108(2):228–36.https://doi.org/10.1093/AJCN/NQY090
X
Referencias
Fiks AG, Gruver RS, Bishop-Gilyard CT, Shults J, Virudachalam S, Suh AW, et al. A Social Media Peer Group for Mothers To Prevent Obesity from Infancy: The Grow2Gether Randomized Trial. Child Obes. 2017;13(5):356–68. https://doi.org/10.1089/CHI.2017.0042
X
Referencias
Thomson JL, Goodman MH, Tussing-Humphreys LM, Landry AS. Infant growth outcomes from birth to 12 months of age: findings from the Delta Healthy Sprouts randomized comparative impact trial. Obes Sci Pract. 2018;4(4):299–307. https://doi.org/10.1002/OSP4.272
X
Referencias
Wasser HM, Thompson AL, Suchindran CM, Goldman BD, Hodges EA, Heinig MJ, et al. Home-based intervention for non-Hispanic black families finds no significant difference in infant size or growth: results from the Mothers & Others randomized controlled trial. BMC Pediatr. 2020;20:1–13. https://doi.org/10.1186/s12887-020-02273-9
X
Referencias
Wen LM, Baur LA, Simpson JM, Rissel C, Wardle K, Flood VM. Effectiveness of home based early intervention on children’s BMI at age 2: randomised controlled trial. The BMJ. 2012;344:e3732. https://doi.org/10.1136/BMJ.E3732
X
Referencias
Wen LM, Baur LA, Simpson JM, Xu H, Hayes AJ, Hardy LL, et al. Sustainability of Effects of an Early Childhood Obesity Prevention Trial Over Time: A Further 3-Year Follow-up of the Healthy Beginnings Trial. JAMA Pediatr. 2015;169(6):543–51. https://doi.org/10.1001/JAMAPEDIATRICS.2015.0258
X
Referencias
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1-7. https://doi.org/10.1186/S12874-018-0611-X
X
Referencias
Salam RA, Padhani ZA, Das JK, Shaikh AY, Hoodbhoy Z, Jeelani SM, et al. Effects of Lifestyle Modification Interventions to Prevent and Manage Child and Adolescent Obesity: A Systematic Review and Meta-Analysis. Nutrients. 2020;12:2208. https://doi.org/10.3390/NU12082208
X
Referencias
Isong IA, Rao SR, Bind MA, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics. 2018;141(1):e20170865. https://doi.org/10.1542/peds.2017-0865
X
Referencias
Andrea SB, Hooker ER, Messer LC, Tandy T, Boone-Heinonen J. Does the association between early life growth and later obesity differ by race/ethnicity or socioeconomic status? A systematic review. Ann Epidemiol. 2017;27(9):583-592. https://doi.org/10.1016/J.ANNEPIDEM.2017.08.019
X
Referencias
Ayala GX, Monge-Rojas R, King AC, Hunter R, Berge JM. Entorno social y obesidad infantil: implicaciones para la investigación y la práctica en Estados Unidos y en los países latinoamericanos. Obes Rev. 2021;22:e13350. https://doi.org/10.1111/OBR.13350
X
Referencias
Iguacel I, Gasch-Gallén Á, Ayala-Marín AM, De Miguel-Etayo P, Moreno LA. Social vulnerabilities as risk factor of childhood obesity development and their role in prevention programs. Int J Obes (Lond). 2021;45:1-11. https://doi.org/10.1038/S41366-020-00697-Y
X
Referencias
Reilly JJ, Martin A, Hughes AR. Early-Life Obesity Prevention: Critique of Intervention Trials During the First One Thousand Days. Curr Obes Rep. 2017;6:127–33. https://doi.org/10.1007/S13679-017-0255-X
X
Referencias
Moreno JM, Collado MC, Larqué E, Leis MR, Sáenz-de-Pipaon M, Moreno LA, et al. Los primeros 1000 días: una oportunidad para reducir la carga de las enfermedades no transmisibles. Nutr Hosp. 2019;36(1):218–32. https://doi.org/10.20960/NH.02453
X
Referencias
Palacios C, Magnus M, Arrieta A, Gallardo H, Tapia R, Espinal C. Obesity in Latin America, a scoping review of public health prevention strategies and an overview of their impact on obesity prevention. Public Health Nutr. 2021;24(15):5142–55. https://doi.org/10.1017/S1368980021001403
X
Referencias
Goldfeld S, Price A, Smith C, Bruce T, Bryson H, Mensah F, et al. Nurse home visiting for families experiencing adversity: A randomized trial. Pediatrics. 2019;143(1): e20181206. https://doi.org/10.1542/peds.2018-1206
X
Referencias
Tiruneh GT, Shiferaw CB, Worku A. Effectiveness and cost-effectiveness of home-based postpartum care on neonatal mortality and exclusive breastfeeding practice in low-and-middle-income countries: A systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19:1–19. https://doi.org/10.1186/s12884-019-2651-6
X
Referencias
Molloy C, Beatson R, Harrop C, Perini N, Goldfeld S. Systematic review: Effects of sustained nurse home visiting programs for disadvantaged mothers and children. J Adv Nurs. 2021;77(1):147–161. https://doi.org/10.1111/JAN.14576
X
Referencias
Turner T, Spruijt-Metz D, Wen CKF, Hingle MD. Prevention and treatment of pediatric obesity using mobile and wireless technologies: a systematic review. Pediatr Obes. 2015;10(6):403–409. https://doi.org/10.1111/IJPO.12002
X
Referencias
Bonvicini L, Pingani I, Venturelli F, Patrignani N, Bassi MC, Broccoli S, et al. Effectiveness of mobile health interventions targeting parents to prevent and treat childhood Obesity: Systematic review. Prev Med Rep. 2022;29:101940. https://doi.org/10.1016/J.PMEDR.2022.101940
X
Referencias
Narzisi K, Simons J. Interventions that prevent or reduce obesity in children from birth to five years of age: A systematic review. Journal of Child Health Care. 2021;25(2):320–334. https://doi.org/10.1177/1367493520917863
X
Referencias
Fowler LA, Grammer AC, Staiano AE, Fitzsimmons-Craft EE, Chen L, Yaeger LH, et al. Harnessing technological solutions for childhood obesity prevention and treatment: a systematic review and meta-analysis of current applications. International Journal of Obesity. 2021 45:5 2021;45:957–981. https://doi.org/10.1038/s41366-021-00765-x
-
Horesh A, Tsur AM, Bardugo A, Twig G. Adolescent and Childhood Obesity and Excess Morbidity and Mortality in Young Adulthood—a Systematic Review. Curr Obes Rep. 2021;10:301–10. https://doi.org/10.1007/s13679-021-00439-9
-
World Health Organization. Obesity and overweight. WHO [Internet] 2023 [Referenced on: 2023, October 15]. Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
-
Lister NB, Baur LA, Felix JF, Hill AJ, Marcus C, Reinehr T, et al. Child and adolescent obesity. Nature Reviews Disease Primers. 2023;9(1):1–19.https://doi.org/10.1038/s41572-023-00435-4
-
Deal BJ, Huffman MD, Binns H, Stone NJ. Perspective: Childhood Obesity Requires New Strategies for Prevention. Advances in Nutrition. 2020;11(5):1071–8. https://doi.org/10.1093/ADVANCES/NMAA040
-
World Health Organization. Noncommunicable diseases: Childhood overweight and obesity [Internet] 2020 [Referenced on: 2023, October 15]. Available at: https://www.who.int/news-room/questions-and-answers/item/noncommunicable-diseases-childhood-overweight-and-obesity
-
Larqué E, Labayen I, Flodmark CE, Lissau I, Czernin S, Moreno LA, et al. From conception to infancy — early risk factors for childhood obesity. Nat Rev Endocrinol. 2019;15:456–78. https://doi.org/10.1038/S41574-019-0219-1
-
United Nations Children’s Fund. Recomendaciones de política pública nacional, estatal y local resumen ejecutivo [Internet] 2019 [Referenced on: 2023, October 15]. Available from: https://www.unicef.org/mexico/media/5326/file/Documento%20de%20recomendaciones.pdf
-
Schwarzenberg SJ, Georgieff MK, Daniels S, Corkins M, Golden NH, Kim JH et al. Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics. 2018;141(2):e20173716. https://doi.org/10.1542/peds.2017-3716
-
Pietrobelli A, Agosti M, MeNu Group. Nutrition in the First 1000 Days: Ten Practices to Minimize Obesity Emerging from Published Science. Int J Environ Res Public Health. 2017;14(12):1491. https://doi.org/10.3390/IJERPH14121491
-
Karacabeyli D, Allender S, Pinkney S, Amed S. Evaluation of complex community-based childhood obesity prevention interventions. Obes Rev. 2018;19(8):1080–92. https://doi.org/10.1111/OBR.12689
-
Hennessy M, Heary C, Laws R, van Rhoon L, Toomey E, Wolstenholme H, et al. The effectiveness of health professional-delivered interventions during the first 1000 days to prevent overweight/obesity in children: A systematic review. Obes Rev. 2019;20(12):1691–707.https://doi.org/10.1111/OBR.12924
-
Blake-Lamb TL, Locks LM, Perkins ME, Woo Baidal JA, Cheng ER, Taveras EM. Interventions for Childhood Obesity in the First 1,000 Days A Systematic Review. Am J Prev Med. 2016;50(6):780–9. https://doi.org/10.1016/J.AMEPRE.2015.11.010
-
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73. https://doi.org/10.7326/M18-0850
-
Zepeda PA, Cárdenas VM, Sifuentes DC. Interventions for early prevention of childhood obesity during the first 1000 days: A scoping review protocol 2023. https://doi.org/10.17605/OSF.IO/5BAMK
-
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616
-
Zepeda PA, Cárdenas VM, Sifuentes DC, Guevara MC. Intervenciones para prevenir la obesidad en los primeros 1000 días: Scoping Review - Mendeley Data V1. https://doi.org/10.17632/zvk4wby72y.1
-
Reifsnider E, McCormick DP, Cullen KW, Todd M, Moramarco MW, Gallagher MR, et al. Randomized Controlled Trial to Prevent Infant Overweight in a High-Risk Population. Acad Pediatr. 2018;18(3):324–33. https://doi.org/10.1016/J.ACAP.2017.12.007
-
McCormick DP, Reyna L, Reifsnider E. Calories, Caffeine and the Onset of Obesity in Young Children. Acad Pediatr. 2020;20(6):801–8. https://doi.org/10.1016/J.ACAP.2020.02.014
-
Gross RS, Mendelsohn AL, Gross MB, Scheinmann R, Messito MJ. Randomized Controlled Trial of a Primary Care-Based Child Obesity Prevention Intervention on Infant Feeding Practices. J Pediatr. 2016;174:171-177. https://doi.org/10.1016/J.JPEDS.2016.03.060
-
Messito MJ, Mendelsohn AL, Katzow MW, Scott MA, Vandyousefi S, Gross RS. Prenatal and Pediatric Primary Care-Based Child Obesity Prevention Program: A Randomized Trial. Pediatrics. 2020;146(4):e20200709. https://doi.org/10.1542/peds.2020-0709
-
Ordway MR, Sadler LS, Holland ML, Slade A, Close N, Mayes LC. A Home Visiting Parenting Program and Child Obesity: A Randomized Trial. Pediatrics. 2018;141(2). https://doi.org/10.1542/PEDS.2017-1076
-
Parat S, Nègre V, Baptiste A, Valensi P, Bertrand AM, Chollet C, et al. Prenatal education of overweight or obese pregnant women to prevent childhood overweight (the ETOIG study): an open-label, randomized controlled trial. Int J Obes (Lond). 2019;43:362–73.https://doi.org/10.1038/S41366-018-0205-Z
-
Fangupo LJ, Heath ALM, Williams SM, Somerville MR, Lawrence JA, Gray AR, et al. Impact of an early-life intervention on the nutrition behaviors of 2-y-old children: a randomized controlled trial. Am J Clin Nutr. 2015;102(3):704–12. https://doi.org/10.3945/AJCN.115.111823
-
Taylor RW, Williams SM, Fangupo LJ, Wheeler BJ, Taylor BJ, Daniels L, et al. Effect of a Baby-Led Approach to Complementary Feeding on Infant Growth and Overweight: A Randomized Clinical Trial. JAMA Pediatr. 2017;171(9):838-846. https://doi.org/10.1001/JAMAPEDIATRICS.2017.1284
-
Taylor RW, Gray AR, Heath ALM, Galland BC, Lawrence J, Sayers R, et al. Sleep, nutrition, and physical activity interventions to prevent obesity in infancy: follow-up of the Prevention of Overweight in Infancy (POI) randomized controlled trial at ages 3.5 and 5 y. Am J Clin Nutr. 2018;108(2):228–36.https://doi.org/10.1093/AJCN/NQY090
-
Fiks AG, Gruver RS, Bishop-Gilyard CT, Shults J, Virudachalam S, Suh AW, et al. A Social Media Peer Group for Mothers To Prevent Obesity from Infancy: The Grow2Gether Randomized Trial. Child Obes. 2017;13(5):356–68. https://doi.org/10.1089/CHI.2017.0042
-
Thomson JL, Goodman MH, Tussing-Humphreys LM, Landry AS. Infant growth outcomes from birth to 12 months of age: findings from the Delta Healthy Sprouts randomized comparative impact trial. Obes Sci Pract. 2018;4(4):299–307. https://doi.org/10.1002/OSP4.272
-
Wasser HM, Thompson AL, Suchindran CM, Goldman BD, Hodges EA, Heinig MJ, et al. Home-based intervention for non-Hispanic black families finds no significant difference in infant size or growth: results from the Mothers & Others randomized controlled trial. BMC Pediatr. 2020;20:1–13. https://doi.org/10.1186/s12887-020-02273-9
-
Wen LM, Baur LA, Simpson JM, Rissel C, Wardle K, Flood VM. Effectiveness of home based early intervention on children’s BMI at age 2: randomised controlled trial. The BMJ. 2012;344:e3732. https://doi.org/10.1136/BMJ.E3732
-
Wen LM, Baur LA, Simpson JM, Xu H, Hayes AJ, Hardy LL, et al. Sustainability of Effects of an Early Childhood Obesity Prevention Trial Over Time: A Further 3-Year Follow-up of the Healthy Beginnings Trial. JAMA Pediatr. 2015;169(6):543–51. https://doi.org/10.1001/JAMAPEDIATRICS.2015.0258
-
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1-7. https://doi.org/10.1186/S12874-018-0611-X
-
Salam RA, Padhani ZA, Das JK, Shaikh AY, Hoodbhoy Z, Jeelani SM, et al. Effects of Lifestyle Modification Interventions to Prevent and Manage Child and Adolescent Obesity: A Systematic Review and Meta-Analysis. Nutrients. 2020;12:2208. https://doi.org/10.3390/NU12082208
-
Fondo de las Naciones Unidas para la Infancia. La obesidad no es una tendencia imparable. Referenced on: November 03, 2023. Available at: https://www.unicef.org/lac/historias/la-obesidad-no-es-una-tendencia-imparable
-
Ríos-Reyna C, Díaz-Ramírez G, Castillo-Ruíz O, Pardo-Buitimea NY, Alemán-Castillo SE. Políticas y estrategias para combatir la obesidad en Latinoamérica. Rev Med Inst Mex Seguro Soc. 2022;60(6):666-674. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10395955/
-
Isong IA, Rao SR, Bind MA, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics. 2018;141(1):e20170865. https://doi.org/10.1542/peds.2017-0865
-
Andrea SB, Hooker ER, Messer LC, Tandy T, Boone-Heinonen J. Does the association between early life growth and later obesity differ by race/ethnicity or socioeconomic status? A systematic review. Ann Epidemiol. 2017;27(9):583-592. https://doi.org/10.1016/J.ANNEPIDEM.2017.08.019
-
Ayala GX, Monge-Rojas R, King AC, Hunter R, Berge JM. Entorno social y obesidad infantil: implicaciones para la investigación y la práctica en Estados Unidos y en los países latinoamericanos. Obes Rev. 2021;22:e13350. https://doi.org/10.1111/OBR.13350
-
Iguacel I, Gasch-Gallén Á, Ayala-Marín AM, De Miguel-Etayo P, Moreno LA. Social vulnerabilities as risk factor of childhood obesity development and their role in prevention programs. Int J Obes (Lond). 2021;45:1-11. https://doi.org/10.1038/S41366-020-00697-Y
-
Reilly JJ, Martin A, Hughes AR. Early-Life Obesity Prevention: Critique of Intervention Trials During the First One Thousand Days. Curr Obes Rep. 2017;6:127–33. https://doi.org/10.1007/S13679-017-0255-X
-
Moreno JM, Collado MC, Larqué E, Leis MR, Sáenz-de-Pipaon M, Moreno LA, et al. Los primeros 1000 días: una oportunidad para reducir la carga de las enfermedades no transmisibles. Nutr Hosp. 2019;36(1):218–32. https://doi.org/10.20960/NH.02453
-
Palacios C, Magnus M, Arrieta A, Gallardo H, Tapia R, Espinal C. Obesity in Latin America, a scoping review of public health prevention strategies and an overview of their impact on obesity prevention. Public Health Nutr. 2021;24(15):5142–55. https://doi.org/10.1017/S1368980021001403
-
Goldfeld S, Price A, Smith C, Bruce T, Bryson H, Mensah F, et al. Nurse home visiting for families experiencing adversity: A randomized trial. Pediatrics. 2019;143(1): e20181206. https://doi.org/10.1542/peds.2018-1206
-
Tiruneh GT, Shiferaw CB, Worku A. Effectiveness and cost-effectiveness of home-based postpartum care on neonatal mortality and exclusive breastfeeding practice in low-and-middle-income countries: A systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19:1–19. https://doi.org/10.1186/s12884-019-2651-6
-
Molloy C, Beatson R, Harrop C, Perini N, Goldfeld S. Systematic review: Effects of sustained nurse home visiting programs for disadvantaged mothers and children. J Adv Nurs. 2021;77(1):147–161. https://doi.org/10.1111/JAN.14576
-
Turner T, Spruijt-Metz D, Wen CKF, Hingle MD. Prevention and treatment of pediatric obesity using mobile and wireless technologies: a systematic review. Pediatr Obes. 2015;10(6):403–409. https://doi.org/10.1111/IJPO.12002
-
Bonvicini L, Pingani I, Venturelli F, Patrignani N, Bassi MC, Broccoli S, et al. Effectiveness of mobile health interventions targeting parents to prevent and treat childhood Obesity: Systematic review. Prev Med Rep. 2022;29:101940. https://doi.org/10.1016/J.PMEDR.2022.101940
-
Narzisi K, Simons J. Interventions that prevent or reduce obesity in children from birth to five years of age: A systematic review. Journal of Child Health Care. 2021;25(2):320–334. https://doi.org/10.1177/1367493520917863
-
Fowler LA, Grammer AC, Staiano AE, Fitzsimmons-Craft EE, Chen L, Yaeger LH, et al. Harnessing technological solutions for childhood obesity prevention and treatment: a systematic review and meta-analysis of current applications. International Journal of Obesity. 2021 45:5 2021;45:957–981. https://doi.org/10.1038/s41366-021-00765-x