Rev Cuid. 2024; 15(2): e3854
Abstract
Introduction: Hospitals serve as important settings for health education initiatives facilitated by technology. Utilizing these resources, healthcare professionals can enhance patient care practices. Objective: This study aims to assess the efficacy of information and communication technologies in enhancing the knowledge of hospitalized patients. Materials and Methods: A systematic review was conducted to address the research question: "Which information and communication technologies effectively improve the knowledge of hospitalized patients?" The search encompassed electronic databases such as Scopus, the National Library of Medicine, Web of Science, Cumulative Index of Nursing and Allied Health Literature, Scientific Electronic Library Online, Cochrane, and Excerpta Medica Database. Gray literature was sourced through Google Scholar. The exposure factor was educational interventions employing information and communication technologies, with the outcome measured as improved knowledge. Only randomized clinical trials in any language were included. Results: A total of 1,153 articles were initially identified, from which four were deemed eligible for inclusion. These studies demonstrated effectiveness in enhancing knowledge through educational interventions utilizing technologies such as video, applications, and concept maps. Discussion: Information and communication technologies have been shown to enhance patient knowledge. Nonetheless, there is a paucity of research exploring hospitals as platforms for technology-mediated educational interventions. Conclusion: Educational interventions employing information and communication technologies in hospital settings effectively enhance patient knowledge.
Key Words: Health Education; Information and Communication Technologies; Health Promotion; Nursing Care.
Resumen
Introducción: El hospital es un escenario para el desarrollo de acciones de educación en salud mediadas por tecnologías. El uso de estos recursos por profesionales puede contribuir a mejores prácticas de salud. Objetivo: Evaluar la eficacia de tecnologías de información y comunicación en la mejora del conocimiento de pacientes hospitalizados. Materiales y Métodos: Revisión sistemática realizada a partir de la pregunta: ¿Qué tecnologías de información y comunicación son eficaces en la mejora del conocimiento de los pacientes hospitalizados? La búsqueda se realizó en las bases de datos Scopus, National Library of Medicine and National Institutes of Health, Web of Science, Cumulative Index of Nursing and Allied Health Literature, Scientific Electronic Library Online, Cochrane y Excerpta Medica Database. Para la búsqueda de literatura gris, se utilizó Google Scholar. El factor de exposición fue la intervención educativa con uso de tecnologías de información y comunicación, y como resultado: mejora del conocimiento. Se incluyeron solo ensayos clínicos aleatorizados, en todos idiomas. Resultados: Se identificaron 1 153 artículos, de los cuales se incluyeron cuatro que revelaron eficacia en la mejora del conocimiento a partir de intervenciones educativas mediadas por tecnología del tipo video, aplicación y mapa conceptual. Discusión: Las tecnologías de información y comunicación mejoran el conocimiento de los pacientes; sin embargo, son pocos los estudios que exploran el hospital como medio para realización de intervenciones educativas mediadas por tecnologías. Conclusión: Las intervenciones educativas con el uso de tecnologías de información y comunicación en el ámbito hospitalario son eficaces para la mejora del conocimiento de pacientes.
Palabras Clave: Educación para la Salud; Tecnologías de la Información y la Comunicación; Promoción de la Salud; Cuidado de Enfermería.
Resumo
Introdução: O hospital é um dos cenários para o desenvolvimento de ações de educação em saúde mediadas por tecnologias. O uso destes recursos pelos profissionais pode coadjuvar em melhores práticas de saúde. Objetivo: Avaliar a eficácia de tecnologias de informação e comunicação na melhora do conhecimento de pacientes hospitalizados. Materiais e Métodos: Revisão sistemática, realizada a partir da questão norteadora: quais tecnologias de informação e comunicação são eficazes na melhora do conhecimento de pacientes hospitalizados? A busca ocorreu nas bases de dados eletrônicas: Scopus; National Library of Medicine and National Institutes of Health; Web of Science; Cumulative Index of Nursing and Allied Health Literature; Scientific Electronic Library Online; Cochrane e Excerpta Medica dataBASE. Para a busca da literatura cinzenta, utilizou-se o Google Scholar. O fator de exposição foi a intervenção educativa com o uso das tecnologias de informação e comunicação, e como desfecho: melhora do conhecimento. Incluíram-se apenas ensaios clínicos randomizados, em todos os idiomas. Resultados: Identificaram-se 1.153 artigos, dos quais foram incluídos quatro que revelaram eficácia sobre melhora do conhecimento a partir de intervenções educativas mediadas por tecnologia do tipo vídeo, aplicativo e mapa conceitual. Discussão: Tecnologias de informação e comunicação melhora o conhecimento dos pacientes, no entanto, são poucos os estudos que exploram o hospital como meio para realização de intervenções educativas mediadas por tecnologias. Conclusão: As intervenções educativas com o uso das tecnologias de informação e comunicação no âmbito hospitalar são eficazes para a melhora do conhecimento dos pacientes.
Palavras-Chave: Educação em Saúde; Tecnologias de Informação e Comunicação; Promoção da Saúde; Cuidados de Enfermagem.
Introduction
In the realm of healthcare, hospitals have become settings for the development of actions utilizing various technologies for health education1,2. Therefore, professionals' sensitivity to the use of Information and Communication Technology (ICT) in healthcare can influence best health practices3.
A study conducted in the United Kingdom emphasizes that information and communication are significant components of interactions between patients and professionals in the emergency sector4. In Brazil, a study supports these findings by highlighting that ICTs are tools used by professionals for health education, providing convenience and greater accessibility to various topics addressed in this work process5.
Advancements in health information technology create opportunities for patients to actively engage in their care. Systematic reviews confirm these findings, showing that technology-based health interventions have had positive effects on patient engagement, behaviors, and knowledge6-8.
Few studies have explored the use of ICTs to improve patient knowledge of health topics during hospitalization7, despite strong guidelines advocating for patient engagement9. Review studies that explored the use of ICTs in hospitals did not specifically address the effectiveness of these technologies aimed at improving patient knowledge10.
Furthermore, available studies touch upon ICT themes but seldom explore their relationship with knowledge and the types and aspects of interventions that yielded positive results. In this context, it becomes relevant to gather and synthesize evidence on the effectiveness of ICTs in improving the knowledge of hospitalized patients to support healthcare systems in Latin America, where challenges persist and resources are limited. Thus, the use of ICTs can assist in improving patient care and the culture of patient safety11,12.
This review aims to provide healthcare professionals, researchers, and policymakers with an overview of interventions aimed at improving knowledge, their procedures, benefits, and application scenarios. Therefore, the objective is to evaluate the effectiveness of information and communication technologies in enhancing the knowledge of hospitalized patients.
Materials and Methods
This systematic literature review was conducted following the Joanna Briggs Institute (JBI) guidelines and registered in the PROSPERO platform under registration CRD42023410493. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was used to report this review13.
The research question was guided by the PICO framework. It was formulated as follows: Population (P) - hospitalized patients; Intervention (I) - information and communication technologies for health education; Comparator (C) - not defined as it varied across studies; and Outcome (O) - improvement in patient knowledge. Based on this framework, the following research question was developed14: Which ICTs are effective in improving the knowledge of hospitalized patients?
Studies in all languages were included if they assessed the effectiveness of ICTs used in hospitals to improve patient knowledge of health topics. Educational interventions using ICTs were required to begin and end in the hospital setting. The thematic focus of interventions was unrestricted, aiming to broaden the analysis on health education in hospitals, an area noted for existing knowledge gaps in the literature10,15. The established outcome was an improvement in patient knowledge. Exclusion criteria encompassed articles on ICT use in other settings, editorials, and letters to the editor.
The search for studies was conducted in April 2023 across the following databases: Scopus; National Library of Medicine and National Institutes of Health (PubMed/PMC); Web of Science; Cumulative Index of Nursing and Allied Health Literature (CINAHL); Scientific Electronic Library Online (SciELO); Cochrane, and Excerpta Medica Database (Embase). Grey literature was searched using Google Scholar.
The keywords from the PICO framework were used to identify controlled vocabulary terms in Health Sciences Descriptors (DeCS), Medical Subject Headings (MeSH), and Emtree. Preliminary searches in databases aimed to identify free vocabulary also used in the literature.
The search strategy developed was tested and approved across all selected databases, described as follows: (("Hospital" OR "Patient Engagement" OR "Patient Involvement" OR "Patient Participation") AND (“Information Technology” OR “Health Information Technology” OR "educational technology" OR "instructional technology") AND (“Knowledge” OR "Education, Health" OR "Health Education" OR "health promotion" OR "patient education")).
Citations and abstracts found were exported to Rayyan QCRI from the Qatar Computing Research Institute16 for removal of duplicate publications. Subsequently, the process of screening titles and abstracts was conducted independently by two reviewers. In cases of doubt or disagreement regarding the inclusion of any material, a third reviewer was consulted. References of included studies were then checked to identify additional studies.
The JBI instrument for data collection and analysis was adapted for this study, with the following data collected: study details (article title, journal, country, language), author/year, study design, objectives, population, sample losses, study period, setting/context, intervention description, comparator, evaluation method (instruments used to measure knowledge), number of sessions/intervention duration, assessment points, findings/conclusions, and contributions to practice.
For the final analysis of articles, the JBI Data Extraction Form for Experimental/Observational Studies was utilized. At this stage, both evaluators independently conducted methodological critical appraisal, considering common conclusions between them.
To synthesize the included articles, the following steps were followed: synthesis of outcomes, extraction of quantitative data, summarization of effect measures, flowchart of article selection in a figure, and presentation of descriptive data in tables14. After analysis, articles were categorized with the following information: country, sample, hospital sector, ICTs, duration and intervention details, technology used in the control and intervention groups, and key results.
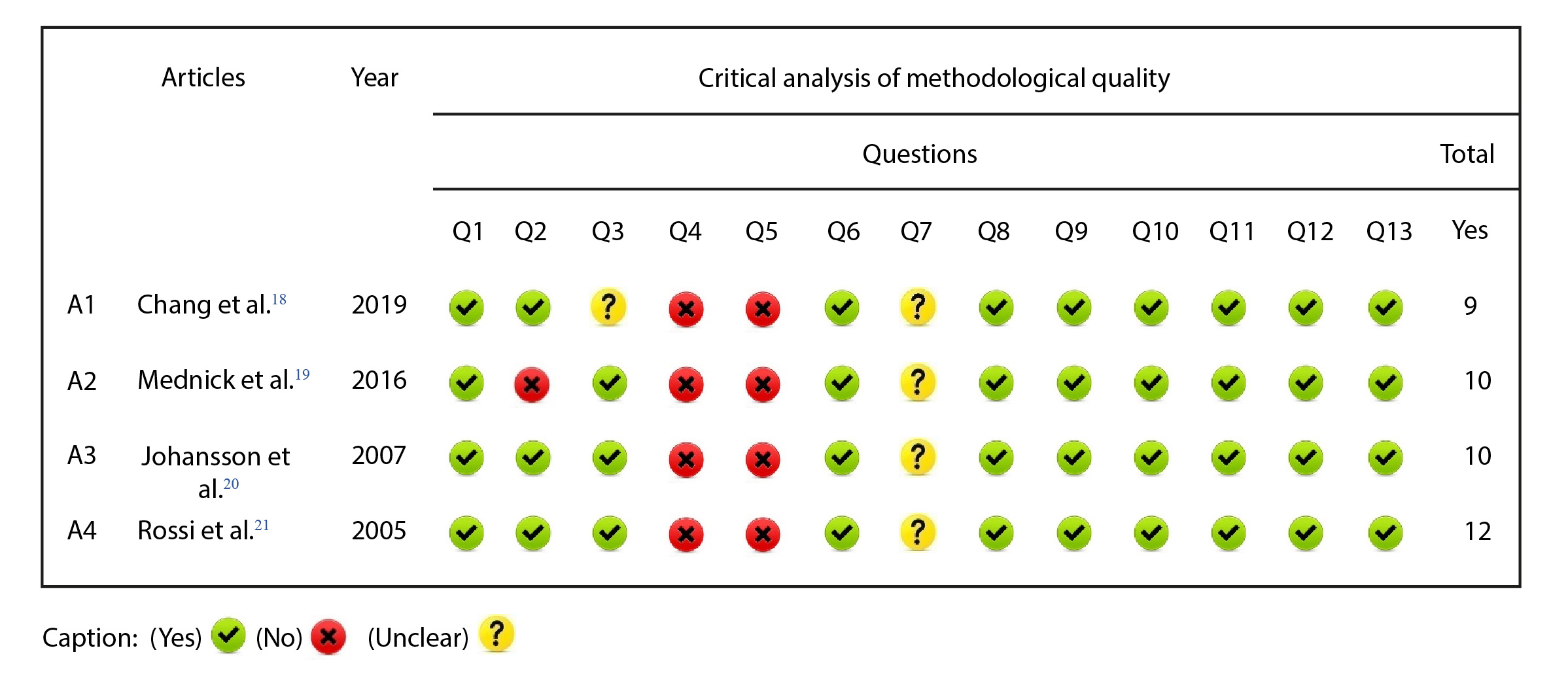
Subsequently, the studies underwent rigorous methodological quality analysis using the JBI critical appraisal checklist for randomized controlled trials, consisting of 13 questions related to internal validity and statistical aspects of the studies. It is noted that all collected data are fully accessible and available for consultation on Figshare17.
Results
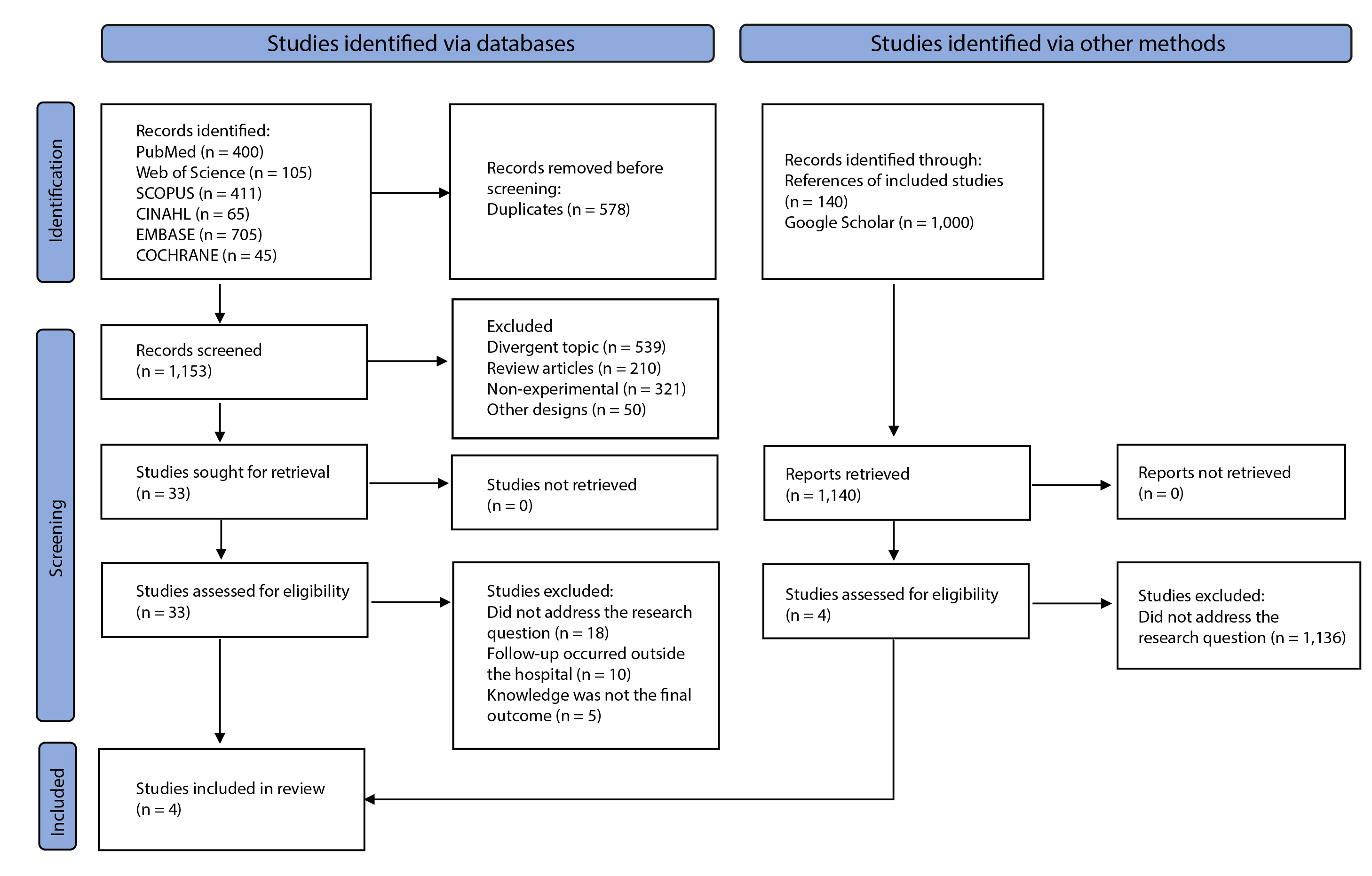
From the search, 2,293 articles were identified, of which 578 were duplicates and 2,265 did not meet the eligibility criteria. Therefore, 37 studies were fully analyzed, and after this stage, a final sample of four studies was selected. The selection process can be observed in the flowchart (Figure 1).
The four articles selected for the final sample are from international journals published in English. The publications originated from Taiwan (1), Canada (1), Finland (1), and the United States (1). The four studies involved approximately 273 patients, predominantly adult females. The follow-up time for interventions ranged from one to 28 days. The following table (Table 1) presents details regarding the characterization of findings.
Table 1. Characterization of studies based on intervention information
X
Table 1. Characterization of studies based on intervention information
| Reference/Country |
Sample |
Hospital sector |
ICTs |
Duration of intervention |
Details of the educational intervention |
Control |
Instrument for measuring knowledge |
Main results |
| Chang et al., 2019 (Taiwan)18 |
70 participants |
Plastic surgery ward |
Mobile application |
An average of 28 days, with intervention at baseline, an average of nine days after and seven days before discharge |
The intervention was carried out by the nurse and mediated by ICT, with the aim of guiding the patient through dressing changes. During the procedure, photographic records of the step-by-step were made using the app, so that the patient could reinforce their knowledge along with the general instructions also present in the technology. |
Brochure |
Wound Care Knowledge Scale and Wound Care Skills Scale |
Knowledge improved in both groups, but the magnitude of the findings was greater in the intervention group (CI = 1.51, p = 0.025). Consequently, dressing change skills were also better in the intervention group (CI = 2.03, p = 0.001). |
| Mednick et al., 2016 (Canada)19 |
78 participants |
Department of Ophthalmology |
Educational video |
It took place in one session. |
The ICT aimed to guide patients through the Fluorescent Retinography (FR) procedure. The intervention was applied at the time of signing the consent form for the examination. The video was about four minutes long and presented information on clinical indications, risks, benefits, and how to administer (FR). |
Standard guidance offered by the ophthalmologist before the procedure |
Knowledge test designed by the authors with six questions and four answer options. |
The intervention group scored better in the knowledge test (84.00% correct) than the control group (73.00% correct). Therefore, there was evidence of efficacy in improving knowledge with the use of video compared to standard guidance (p=0.001). |
| Johansson et al.,2007 (Finland)20 |
123 participants |
Surgical clinic |
Concept map |
It took place in one session, lasting one hour, two weeks before admission for orthopedic surgery. |
The intervention was applied by a nurse who had previously been trained to build a concept map with the aim of guiding patients through orthopedic surgery. The facilitator sat next to the patient and discussed functional, experiential, ethical, social, and financial issues associated with the surgery. As the intervention unfolded, the concept map was constructed and then made available to the patient. |
Routine unit orientation |
Orthopedic Patient Knowledge Questionnaire (OPKQ) Modified Empowerment Questionnaire (MEQ) |
Patients who received pre-admission health education had higher knowledge scores in both assessments, at admission and discharge (M = 4.05 > 4.30, improving 0.25, p < 0.002). |
| Rossi et al.,2005 (United States)21 |
150 participants |
Health education sector in the hospital |
Educational video |
It took place in one session |
The intervention was mediated using an educational video aimed at guiding patients through knee arthroscopy. The ICT was developed by the American Academy of Orthopedic Surgeons and lasted 12 minutes. After viewing the video, the patient asked questions of the intervention facilitator. |
Routine unit orientation |
Knowledge assessment questionnaire constructed by the authors |
Patients in the intervention group obtained an average knowledge score of 81.00% in the knowledge test (SD=10.50%), while patients in the control group scored 71.10% (SD=14.10%). It was therefore observed that the video was effective in improving knowledge about the surgery (p=0.002) |
ICT: Information and communication technology.
Regarding the study population, only one study19 had a majority of elderly individuals over 65 years old. The others were conducted with an adult population between 18 and 57 years old. Educational attainment was reported in three studies18,20,21, with a predominance of individuals having up to 12 years of schooling. No statistical associations were established between educational attainment and improvements in knowledge.
No cognitive assessment instruments were used to evaluate patients included in the studies. Additionally, sample losses were not significant, which may be attributed to the timing of the interventions, predominantly occurring in a single session with evaluations over a short period of time (up to 28 days).
Regarding educational interventions, most took the form of individual counseling and discussions with patients. Printed resources such as concept maps19, audiovisual materials like videos19,21, and digital technologies18 were employed. Among the topics covered in the educational interventions were instructions aimed at improving knowledge about wound care for home follow-up and aspects related to surgical procedures, fluorescent retinography, orthopedic surgery, and knee arthroscopy, which participants were to undergo. Regarding the professional who conducted the intervention, two studies18,20 reported the involvement of nursing professionals, while in the others, the category was not specified. The rigorous analysis of methodological quality of the studies can be observed in Figure 2.
The method for sequence generation and allocation concealment of patients was not clearly described in the findings of some studies, nor was the blinding of outcome assessment for defined outcomes. This is attributed to the educational intervention being conducted at the bedside. Additionally, some studies exhibited a potentially high risk of bias due to insufficient description of the knowledge assessment methods.
Discussion
Findings demonstrated that the use of ICTs to enhance knowledge in hospitals is highly promising. However, few studies explore these spaces as a means for conducting educational interventions mediated by technology. Conversely, hospitals still serve as places where participants are enrolled for follow-up interventions that take place in other settings.
Within the hospital setting, this idealization is reaffirmed by the Budapest Declaration, emphasizing the relevance of active patient profiles in tertiary care sectors and the improvement in the proposal and quality of health information, communication, and education programs10. Despite the existence of international guidelines9,22, few studies have explored hospitalized patient knowledge as a strategy to enhance participation and self-care during hospitalization.
In the studies included in this review, the use of digital technologies such as mobile applications and videos stood out. These resources proved effective in enhancing patient knowledge. Digital tools are generally well-received due to their ease of use, integration of visual and auditory resources, and other features that enhance accessibility23. Other studies using mobile applications for health interventions highlight positive impacts and efficacy in health contexts24-26.
The use of educational interventions through smartphones aligns with the increasing number of individuals seeking health information via mobile devices. It is believed that the functionalities of these apps possess important attributes for transforming healthcare practices, resulting in improved individual knowledge10,27.
A noteworthy point was the use of theoretical frameworks for the development and application of ICTs. In this study, the self-regulation theory, which is based on self-monitoring, self-judgment, and self-reaction28 was applied. The use of this framework facilitated goal setting and strategy definition within the app to promote wound care self-management. However, only this study utilized a theoretical framework to underpin the educational intervention.
In studies using video to guide patients through surgical procedures, the influence of this resource on knowledge retention was evaluated compared to routine service guidance. Findings indicated that the intervention group achieved better knowledge retention among participants19,21.
Another highlighted finding was patient satisfaction with ICT use. A study included in the review evaluated this outcome and demonstrated satisfaction among most participants in the intervention group19. These findings align with other systematic reviews on health technologies based on educational videos, which show their significant role in education, self-management, satisfaction, and improvements in patients' quality of life29,30.
Overall, studies underscore that the use of videos and mobile applications improves patient knowledge, satisfaction, and accessibility, promotes active participation, and facilitates more effective communication during hospitalization31,32. In addition to digital technologies, one study in this review applied a printed technology known as a concept map. This visual tool illustrates relationships between ideas and concepts, aiding in organizing and structuring knowledge and showing interconnections among different pieces of information33.
Research evaluating the use of concept maps for patient health education found that they significantly contributed to surgical patients' understanding of procedures22. This aligns with studies demonstrating that concept maps are widely used for teaching and learning, encouraging active participation and providing a comprehensive view of information34,35.
It is crucial to emphasize the role of healthcare professionals as mediators of intervention. In all studies in this review, a professional was involved in the ICT application process, with nurses predominantly featured18,19,21. These findings support the nurse's role as an educator and underscore the importance of a multidisciplinary team in the educational process7.
Another relevant point was the measurement of patient knowledge and the evaluation of instruments. In two studies in this review, the authors developed their own instruments without reporting their validation, potentially compromising the internal validity of the findings19,21. Using validated instruments ensures that the information obtained is reliable and contributes to better clinical outcomes35.
The review's limitations relate to the heterogeneity of the studies, which precluded meta-analysis execution, emphasizing the need to interpret findings with caution. Although educational interventions were heterogeneous, differences among the included studies should be noted. Some studies defined a small sample size and demonstrated less rigorous data analysis, challenging result validity.
Furthermore, this review provides valuable insights into intervention strategies that have proven effective in the hospital setting. Thus, its results can guide future interventions using technology to enhance patient knowledge about their care during hospitalization.
Conclusion
Educational interventions using ICTs in the hospital setting effectively improve the knowledge of hospitalized patients, resulting in patient satisfaction, skill acquisition, and reduced anxiety among patients.
However, despite the numerous benefits of ICTs, it is important to emphasize that ICT implementation during hospitalization requires behavioral changes from both professionals and patients towards health education. Moreover, it is crucial to ensure that ICTs are used as a tool to support care, maintaining close and empathetic communication between professionals, patients, and their families. Additionally, the future evaluation of cost-effectiveness of these interventions in hospital services is essential.
Based on the findings, this study provides guidance for professionals by offering a theoretical framework grounded in scientific evidence for conducting health education with hospitalized patients, empowering them regarding their health issues. For researchers, there is a highlighted need for well-designed randomized clinical trials on the effectiveness of educational interventions conducted in the hospital setting. Furthermore, the evaluation of the cost-effectiveness of these interventions for services is paramount. For managers and policymakers, educational interventions are recommended as effective means to improve patient knowledge and subsequent participation in healthcare. These interventions are also noted for their low or no implementation costs and their potential for patient adherence in healthcare institutions.
Conflict of Interest: The authors declare no conflict of interest.
Financing: None.
References
X
Referencias
Fontenele NAO, Ximenes MAM, Brandão MGSA, Fernandes CS, Galindo Neto NM, Carvalho REFL, et al. Creation and validation of a serial album for the prevention of Pressure Ulcer: a methodological study. Rev Bras Enferm. 2021;74(3):e20201060. https://doi.org/10.1590/0034-7167-2020-1060
X
Referencias
Merhy EE, Chakkour M, Stéfano E, Stéfano ME, Santos CM, Rodrigues RA. Em busca de ferramentas analisadoras das tecnologias em saúde: a informação e o dia a dia de um serviço, interrogando e gerindo trabalho em saúde. In: Merhy EE, Onocko R, organizadores. Agir em saúde: um desafio para o público. Hucitec; 2006. p. 113-150. https://digitalrepository.unm.edu/lasm_pt/326/
X
Referencias
Prades J, Coll-Ortega C, Dal Lago L, Goffin K, Javor E, Lombardo C, de Munter J, Ponce J, Regge D, Salazar R, Valentini V, Borras JM. Use of information and communication technologies (ICTs) in cancer multidisciplinary team meetings: an explorative study based on EU healthcare professionals. BMJ Open. 2022; 6;12(10):e051181. https://doi.org/10.1136/bmjopen-2021-051181
X
Referencias
Ahmad N, Atoum I, Khan J, Alqahhas Y. ICT Application and Use in Health Sciences Research at the Global Level: A Scientometric Study. Healthcare (Basel). 2022 Sep 5;10(9):1701. https://doi.org/10.3390/healthcare10091701
X
Referencias
Roberts S, Chaboyer W, Gonzalez, R. et al. Using technology to engage hospitalised patients in their care: a realist review. BMC Health Serv Res. 2017;17, 388. https://doi.org/10.1186/s12913-017-2314-0
X
Referencias
Ximenes MAM, Brandão MGSA, Araújo TM, Galindo Neto NM, Barros LM, Caetano JÁ. Efetividade de intervenções educativas para prevenção de quedas: revisão sistemática. Texto Contexto Enferm. 2021; 30:e20200558. https://doi.org/10.1590/1980-265X-TCE-2020-0558
X
Referencias
Prey JE, Woollen J, Wilcox L, Sackeim AD, Hripcsak G, Bakken S, et al. Patient engagement in the inpatient setting: a systematic review. Journal of the American Medical Informatics Association. 2014;21(4):742–50. https://doi.org/10.1136/amiajnl-2013-002141
X
Referencias
Ximenes MAM. Desenvolvimento e validação de tecnologia digital para educação em saúde do paciente sobre prevenção de quedas no hospital. Dissertação (Mestrado em Enfermagem). Universidade Federal do Ceará, Faculdade de Farmácia, Odontologia e Enfermagem, Programa de Pós Graduação em Enfermagem, Fortaleza, 2022. http://repositorio.ufc.br/handle/riufc/64059
X
Referencias
Mendonça RR, Salvador DLVF, Mata TCF da, Nakasima PAM, Derenzo N, Covre ER, et al. Tecnologias Da Informação E Comunicação: Visão Dos Profissionais Do Atendimento Móvel De Urgência E Emergência. Cogitare Enferm. 2022;27:e81985. https://doi.org/10.5380/ce.v27i0.81985
X
Referencias
Camacho-Rodríguez DE, Carrasquilla-Baza DA, Domínguez-Cancino KA, Palmieri PA. Patient Safety Culture in Latin American Hospitals: A Systematic Review with Meta-Analysis. International journal of environmental research and public health. 2022;19(21):14380. https://doi.org/10.3390/ijerph192114380
X
Referencias
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29;372:n71. https://doi.org/10.1136/bmj.n71
X
Referencias
Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7(7):CD012221. https://doi.org/10.1002/14651858.CD012221.pub2
X
Referencias
Chang HY, Hou YP, Yeh FH, Lee SS. The impact of an mHealth app on knowledge, skills and anxiety about dressing changes: A randomized controlled trial. J Adv Nurs. 2020;76(4):1046-1056. https://doi.org/10.1111/jan.14287
X
Referencias
Mednick Z, Irrcher I, Hopman WM, Sharma S. Assessing a narrated white board animation as part of the consent process for intravenous fluorescein angiography: a randomized educational study. Can J Ophthalmol. 2016;51(6):471-475. https://doi.org/10.1016/j.jcjo.2016.04.023
X
Referencias
Johansson K, Salanterä S, Katajisto J. Empowering orthopaedic patients through preadmission education: results from a clinical study. Patient Educ Couns. 2007;66(1):84-91. https://doi.org/10.1016/j.pec.2006.10.011
X
Referencias
Liverpool S, Mota CP, Sales CMD, Cus A, Carletto S, Hancheva C, et al. Engaging Children and Young People in Digital Mental Health Interventions: Systematic Review of Modes of Delivery, Facilitators, and Barriers. J Med Internet Res. 2020;22(6):e16317.https://doi.org/10.2196/16317
X
Referencias
Melia R, Francis K, Hickey E, Bogue J, Duggan J, O'Sullivan M, et al. Mobile Health Technology Interventions for Suicide Prevention: Systematic Review. JMIR Mhealth Uhealth. 2020;15;8(1):e12516. https://doi.org/10.2196/12516
X
Referencias
Currie CL, Larouche R, Voss ML, Trottier M, Spiwak R, Higa E, et al. Effectiveness of Live Health Professional-Led Group eHealth Interventions for Adult Mental Health: Systematic Review of Randomized Controlled Trials. J Med Internet Res. 2022;11;24(1):e27939. https://doi.org/10.2196/27939
X
Referencias
Al-Arkee S, Mason J, Lane DA, Fabritz L, Chua W, Haque MS, et al. Mobile Apps to Improve Medication Adherence in Cardiovascular Disease: Systematic Review and Meta-analysis. J Med Internet Res. 2021;23(5):e24190. https://doi.org/10.2196/24190
X
Referencias
Paula TR, Menezes AP, Guedes NG, Silva VM, Cardoso MVLML, Ramos ES. Effectiveness of mobile applications for behavioral changes in health: a systematic review. Rev Rene. 2020;21:e43845. https://doi.org/10.15253/2175-6783.20202143845
X
Referencias
Fan Y, van der Graaf J, Lim L, Raković M, Singh S, Kilgour J et al. Para investigar a validade da medição da aprendizagem auto-regulada com base em dados de rastreamento. Metacognição Learning. 2022;17:949–987. https://doi.org/10.1007/s11409-022-09291-1
X
Referencias
Tom K, Phang PT. Effectiveness of the video medium to supplement preoperative patient education: A systematic review of the literature. Patient Educ Couns. 2022;105(7):1878-1887. https://doi.org/10.1016/j.pec.2022.01.013
X
Referencias
Acuna N, Vento I, Alzate-Duque L, Valera P. Harnessing Digital Videos to Promote Cancer Prevention and Education: A Systematic Review of the Literature from 2013-2018. J Cancer Educ. 2020;35(4):635-642. https://doi.org/10.1007/s13187-019-01624-0
X
Referencias
Aardoom JJ, Hilt AD, Woudenberg T, Chavannes NH, Atsma DE. A Preoperative Virtual Reality App for Patients Scheduled for Cardiac Catheterization: Pre-Post Questionnaire Study Examining Feasibility, Usability, and Acceptability. JMIR Cardio. 2022;22;6(1):e29473. https://doi.org/10.2196/29473
X
Referencias
Lieser T, Huang Y, Sezgin E. The Current State of Mobile Apps Owned by Large Pediatric Hospitals in the United States: Systematic Search and Analysis on Google Play and Apple App Stores. JMIR Pediatr Parent. 2022;6;5(4):e38940. https://doi.org/10.2196/38940
X
Referencias
Mukhopadhyay K, Mukherjee S, Dhok A, Chatterjee C, Ghosh J. Use of concept map as a reinforcement tool in undergraduate curriculum: An analytical study. J Adv Med Educ Prof. 2019;7(3):118-122. https://doi.org/10.30476/JAMP.2019.74920
X
Referencias
Aliyari S, Pishgooie AH, Abdi A, Mazhari MS, Nazari MR. Comparing two teaching methods based on concept map and lecture on the level of learning in basic life support. Nurse Educ Pract. 2019;38:40-44. https://doi.org/10.1016/j.nepr.2019.05.008
-
Fontenele NAO, Ximenes MAM, Brandão MGSA, Fernandes CS, Galindo Neto NM, Carvalho REFL, et al. Creation and validation of a serial album for the prevention of Pressure Ulcer: a methodological study. Rev Bras Enferm. 2021;74(3):e20201060. https://doi.org/10.1590/0034-7167-2020-1060
-
Merhy EE, Chakkour M, Stéfano E, Stéfano ME, Santos CM, Rodrigues RA. Em busca de ferramentas analisadoras das tecnologias em saúde: a informação e o dia a dia de um serviço, interrogando e gerindo trabalho em saúde. In: Merhy EE, Onocko R, organizadores. Agir em saúde: um desafio para o público. Hucitec; 2006. p. 113-150. https://digitalrepository.unm.edu/lasm_pt/326/
-
Prades J, Coll-Ortega C, Dal Lago L, Goffin K, Javor E, Lombardo C, de Munter J, Ponce J, Regge D, Salazar R, Valentini V, Borras JM. Use of information and communication technologies (ICTs) in cancer multidisciplinary team meetings: an explorative study based on EU healthcare professionals. BMJ Open. 2022; 6;12(10):e051181. https://doi.org/10.1136/bmjopen-2021-051181
-
Blackburn J, Ousey K, Goodwin E. Information and communication in the emergency department. Int Emerg Nurs. 2019;42:30-35. https://doi.org/10.1016/j.ienj.2018.07.002
-
Ahmad N, Atoum I, Khan J, Alqahhas Y. ICT Application and Use in Health Sciences Research at the Global Level: A Scientometric Study. Healthcare (Basel). 2022 Sep 5;10(9):1701. https://doi.org/10.3390/healthcare10091701
-
Roberts S, Chaboyer W, Gonzalez, R. et al. Using technology to engage hospitalised patients in their care: a realist review. BMC Health Serv Res. 2017;17, 388. https://doi.org/10.1186/s12913-017-2314-0
-
Ximenes MAM, Brandão MGSA, Araújo TM, Galindo Neto NM, Barros LM, Caetano JÁ. Efetividade de intervenções educativas para prevenção de quedas: revisão sistemática. Texto Contexto Enferm. 2021; 30:e20200558. https://doi.org/10.1590/1980-265X-TCE-2020-0558
-
Prey JE, Woollen J, Wilcox L, Sackeim AD, Hripcsak G, Bakken S, et al. Patient engagement in the inpatient setting: a systematic review. Journal of the American Medical Informatics Association. 2014;21(4):742–50. https://doi.org/10.1136/amiajnl-2013-002141
-
Mossey PA, Petersen PE. Budapest Declaration: IADR-GOHIRA®. J Dent Res. 2014;93(7 Suppl):120S-121S. https://doi.org/10.1177/0022034514527972
-
Ximenes MAM. Desenvolvimento e validação de tecnologia digital para educação em saúde do paciente sobre prevenção de quedas no hospital. Dissertação (Mestrado em Enfermagem). Universidade Federal do Ceará, Faculdade de Farmácia, Odontologia e Enfermagem, Programa de Pós Graduação em Enfermagem, Fortaleza, 2022. http://repositorio.ufc.br/handle/riufc/64059
-
Mendonça RR, Salvador DLVF, Mata TCF da, Nakasima PAM, Derenzo N, Covre ER, et al. Tecnologias Da Informação E Comunicação: Visão Dos Profissionais Do Atendimento Móvel De Urgência E Emergência. Cogitare Enferm. 2022;27:e81985. https://doi.org/10.5380/ce.v27i0.81985
-
Camacho-Rodríguez DE, Carrasquilla-Baza DA, Domínguez-Cancino KA, Palmieri PA. Patient Safety Culture in Latin American Hospitals: A Systematic Review with Meta-Analysis. International journal of environmental research and public health. 2022;19(21):14380. https://doi.org/10.3390/ijerph192114380
-
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29;372:n71. https://doi.org/10.1136/bmj.n71
-
Oliveira AWC. Recuperação da informação em saúde: construção, modelos e estratégias. ConCI: Convergências em Ciência da Informação, 2020;3(2):100-134. https://doi.org/10.33467/conci.v3i2.13447
-
Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;7(7):CD012221. https://doi.org/10.1002/14651858.CD012221.pub2
-
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4
-
Fontenele NAO, Ximenes MAM, Brandão MGSA; Lima ETF, Gomes SR, Brasil CAR, et al. Systematic review data analysis. figshare. 2024. https://doi.org/10.6084/m9.figshare.25466389.v1
-
Chang HY, Hou YP, Yeh FH, Lee SS. The impact of an mHealth app on knowledge, skills and anxiety about dressing changes: A randomized controlled trial. J Adv Nurs. 2020;76(4):1046-1056. https://doi.org/10.1111/jan.14287
-
Mednick Z, Irrcher I, Hopman WM, Sharma S. Assessing a narrated white board animation as part of the consent process for intravenous fluorescein angiography: a randomized educational study. Can J Ophthalmol. 2016;51(6):471-475. https://doi.org/10.1016/j.jcjo.2016.04.023
-
Johansson K, Salanterä S, Katajisto J. Empowering orthopaedic patients through preadmission education: results from a clinical study. Patient Educ Couns. 2007;66(1):84-91. https://doi.org/10.1016/j.pec.2006.10.011
-
Rossi MJ, Guttmann D, MacLennan MJ, Lubowitz JH. Video informed consent improves knee arthroscopy patient comprehension. Arthroscopy. 2005;21(6):739-43. https://doi.org/10.1016/j.arthro.2005.02.015
-
World Health Organization. Global patient safety action plan 2021–2030 towards zero patient harm in health care. First Draft. [Internet] 2020 [Cited: Sept 21, 2023]. https://www.who.int/teams/integrated-health-services/patient-safety/policy/global-patient-safety-action-plan
-
Liverpool S, Mota CP, Sales CMD, Cus A, Carletto S, Hancheva C, et al. Engaging Children and Young People in Digital Mental Health Interventions: Systematic Review of Modes of Delivery, Facilitators, and Barriers. J Med Internet Res. 2020;22(6):e16317.https://doi.org/10.2196/16317
-
Melia R, Francis K, Hickey E, Bogue J, Duggan J, O'Sullivan M, et al. Mobile Health Technology Interventions for Suicide Prevention: Systematic Review. JMIR Mhealth Uhealth. 2020;15;8(1):e12516. https://doi.org/10.2196/12516
-
Currie CL, Larouche R, Voss ML, Trottier M, Spiwak R, Higa E, et al. Effectiveness of Live Health Professional-Led Group eHealth Interventions for Adult Mental Health: Systematic Review of Randomized Controlled Trials. J Med Internet Res. 2022;11;24(1):e27939. https://doi.org/10.2196/27939
-
Al-Arkee S, Mason J, Lane DA, Fabritz L, Chua W, Haque MS, et al. Mobile Apps to Improve Medication Adherence in Cardiovascular Disease: Systematic Review and Meta-analysis. J Med Internet Res. 2021;23(5):e24190. https://doi.org/10.2196/24190
-
Paula TR, Menezes AP, Guedes NG, Silva VM, Cardoso MVLML, Ramos ES. Effectiveness of mobile applications for behavioral changes in health: a systematic review. Rev Rene. 2020;21:e43845. https://doi.org/10.15253/2175-6783.20202143845
-
Fan Y, van der Graaf J, Lim L, Raković M, Singh S, Kilgour J et al. Para investigar a validade da medição da aprendizagem auto-regulada com base em dados de rastreamento. Metacognição Learning. 2022;17:949–987. https://doi.org/10.1007/s11409-022-09291-1
-
Tom K, Phang PT. Effectiveness of the video medium to supplement preoperative patient education: A systematic review of the literature. Patient Educ Couns. 2022;105(7):1878-1887. https://doi.org/10.1016/j.pec.2022.01.013
-
Acuna N, Vento I, Alzate-Duque L, Valera P. Harnessing Digital Videos to Promote Cancer Prevention and Education: A Systematic Review of the Literature from 2013-2018. J Cancer Educ. 2020;35(4):635-642. https://doi.org/10.1007/s13187-019-01624-0
-
Aardoom JJ, Hilt AD, Woudenberg T, Chavannes NH, Atsma DE. A Preoperative Virtual Reality App for Patients Scheduled for Cardiac Catheterization: Pre-Post Questionnaire Study Examining Feasibility, Usability, and Acceptability. JMIR Cardio. 2022;22;6(1):e29473. https://doi.org/10.2196/29473
-
Lieser T, Huang Y, Sezgin E. The Current State of Mobile Apps Owned by Large Pediatric Hospitals in the United States: Systematic Search and Analysis on Google Play and Apple App Stores. JMIR Pediatr Parent. 2022;6;5(4):e38940. https://doi.org/10.2196/38940
-
Evans T, Jeong I. Concept maps as assessment for learning in university mathematics. Educ Stud Math. 2023;113:475–498.https://doi.org/10.1007/s10649-023-10209-0
-
Mukhopadhyay K, Mukherjee S, Dhok A, Chatterjee C, Ghosh J. Use of concept map as a reinforcement tool in undergraduate curriculum: An analytical study. J Adv Med Educ Prof. 2019;7(3):118-122. https://doi.org/10.30476/JAMP.2019.74920
-
Aliyari S, Pishgooie AH, Abdi A, Mazhari MS, Nazari MR. Comparing two teaching methods based on concept map and lecture on the level of learning in basic life support. Nurse Educ Pract. 2019;38:40-44. https://doi.org/10.1016/j.nepr.2019.05.008