Body mass index associated with characteristics of postpartum patients and newborns
DOI:
https://doi.org/10.15649/cuidarte.v10i2.678Keywords:
Body Mass Index, Obesity, Infant, Newborn, Pregnant Women, Obstetric NursingAbstract
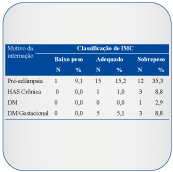
Introduction: An inadequate pregestational Body Mass Index (BMI) leads to maternal/fetal risks. Objectives: To identify the pregestational BMI to link it to the sociodemographic and obstetrical data of postpartum patients as well as to identify how the pregestational BMI and weight gain during pregnancy can be related to the characteristics of newborns. Materials and Methods: A quantitative, descriptive study was conducted in a referral hospital for 187 pairs. The data were collected from the maternity notes and the Certificates of Live Birth. Due to the absence of Gaussian distribution, continuous variables were compared using non-parametric tests (Mann-Whitney or Kruskal-Wallis). Paired samples were compared using the Wilcoxon test for paired data. Fisher’s exact test or Pearson’s chi-square test were used for comparing categorical variables. Results: Pregestational BMI ranged from 16 to 53kg/m², mean 25.0 ±5.9kg/m²; 41.2% overweight and obese women; the average of pregestational weight gain was 11Kg ±30Kg; mean age was 26 years. A progressive weight gain was observed in relation to the increase in age (P=0.009); obese women were more likely to be hospitalized for Gestational Hypertensive Syndrome (P=0.003) and Chronic Hypertension (P=0.026); among women with a high BMI, 24.0% were primiparous while 23.5% were multiparous; the average weight of newborns was 3146.8g ±559.7g. Newborn weight of obese women was higher (P=0.0034). A positive correlation was observed between maternal pregestational BMI and the newborn weight at birth (rho–0.219; P=0.003). Discussion and Conclusions: The assessment of the nutritional status should be made during the planning stage of gestation in order to prevent future complications.
Como citar este artigo: Tresso BD, Tavares BB. Índice de massa corporal associado às caractéristicas das puérperas e dos neonatos. Rev Cuid. 2019; 10(2): e678. http://dx.doi.org/10.15649/cuidarte.v10i2.678
References
Ministério da Saúde, Vigitel. Brasília 2017. 70 p. [acesso em 2017 Ago 16]. Vigitel Brasil 2015- Saúde Suplementar: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico [recurso eletrônico]. Disponível em: http://www.ans.gov.br/images/stories/Materiais_para_pesquisa/Materiais_por_assunto/2015_vigitel.pdf
Wilson RM, Messaoudi I. The impact of maternal obesity during pregnancy on offspring immunity. Mol Cell Endocrinol. 2015; 418(2): 134-42. https://doi.org/10.1016/j.mce.2015.07.028
Mahizir D, Briffa JF, Hryciw DH, Wadley GD, Moritz KM, Wlodek ME. Maternal obesity in females born small: Pregnancy complications and offspring disease risk. Mol Nutr Food Res. 2016; 60(1): 8-17. https://doi.org/10.1002/mnfr.201500289
Mission JF, Marshall NE, Caughey AB. Pregnancy risks associated with obesity. Obstet Gynecol Clin North Am. 2015; 42(2): 335-53. https://doi.org/10.1016/j.ogc.2015.01.008
Downs DS. Obesity in Special Populations: Pregnancy. Prim Care. 2016; 43(1): 109-20. https://doi.org/10.1016/j.pop.2015.09.003
Ferreira RAB, Benicio MHDA. Obesidade em mulheres brasileiras: associação com paridade e nível socioeconômico. Rev Panam Salud Publica. 2015; 37(4/5): 337-42.
Pakniat H, Mohammadi F, Ranjkesh F. The Impact of Body Mass Index on Pregnancy Outcome. J Midwifery Reprod Health. 2015; 3(2): 361-7.
Santangeli L, Sattar N, Huda SS. Impact of maternal obesity on perinatal and childhood outcomes. Best Pract Res Clin Obstet Gynaecol. 2015; 29(3): 438-48. https://doi.org/10.1016/j.bpobgyn.2014.10.009
Thomas H. Maternal obesity affects neonatal adipogenesis. Nature Reviews Endocrinology Published online. 2015. https://doi.org/10.1038/nrendo.2015.225
Ministério da Saúde, Brasil. Secretaria de Atenção à Saúde. Atenção ao pré-natal de baixo risco. Brasília (DF): Editora do Ministério da Saúde. 2013; p.78.
Carlhäll S, Bladh M, Brynhildsen J, Claesson IM, Josefsson A, Sydsjö G, et al. Maternal obesity (Class I-III), gestational weight gain and maternal leptin levels during and after pregnancy: a prospective cohort study. BMC Obes. 2016; 3: 28. https://doi.org/10.1186/s40608-016-0108-2
Cresswell JA, Campbell OM, De Silva MJ, Slaymaker E, Filippi V. Maternal obesity and Caesarean delivery in sub-Saharan Africa. Trop Med Int Health. 2016; 21: 879-85. https://doi.org/10.1111/tmi.12713
Diemert A, Lezius S, Pagenkemper M, Hansen G, Drozdowska A, Hecher K, et al. Maternal nutrition, inadequate gestational weight gain and birth weight: results from aprospective birth cohort. BMC Pregnancy Childbirth. 2016; 16: 224. https://doi.org/10.1186/s12884-016-1012-y
Zanardo V, Mazza A, Parotto M, Scambia G, Straface G. Gestational weight gain and fetal growth in underweight women. Italian Journal of Pediatrics. 2016; 42:74. https://doi.org/10.1186/s13052-016-0284-1
Nicácio TS, Alves VM, Oliveira RMS, Pereira Netto M. Análise histórica do atendimento pré-natal e condições de saúde de gestantes atendidas por uma unidade básica de saúde de Juiz de Fora. JMPHC. 2016; 7(1): 150.
Ferreira RAB, Benicio MHDA. Obesidade em mulheres brasileiras: associação com paridade e nível socioeconômico. Rev Panam Salud Publica. 2015; 37(4/5): 337-42.
Ministério da Saúde, Vigitel. [homepage na internet]. Brasília (DF); 2016. [acesso em 2017 Jul 28]. Vigitel Brasil 2016 - Hábitos dos brasileiros impactam no crescimento da obesidade e aumenta prevalência de diabetes e hipertensão; [aproximadamente 44 telas]. Disponível em: https://www.endocrino.org.br/media/uploads/PDFs/vigitel.pdf
Nascimento IB do, Barbosa WS, Schneider L, Cipriano J, Bollmann da ACM, Silva JC. Identificar a influência da obesidade nos desfechos obstétricos. Arq. Catarin Med. 2017; 46(2): 97-107.
Abacasis MP. A gravidez, o aumento de peso e o acompanhamento nutricional: Custos e benefícios [tese]. Faculdade de Medicina de Lisboa; 2015.
Papachatzi E, Paparrodopoulos S, Papadopoulos V, Dimitriou G, Vantarakis A. Pre-pregnancy maternal obesity in Greece: A case-control analysis. Early Hum Dev. 2016; 93: 57-61. https://doi.org/10.1016/j.earlhumdev.2015.12.006
Xie YJ, Peng R, Han L, Zhou X, Xiong Z, Zhang Y, et al. Associations of neonatal high birth weight with maternal pre-pregnancy body mass index and gestational weight gain: a case-control study in women from Chongqing, China. BMJ Open. 2016; 6(8): e010935. https://doi.org/10.1136/bmjopen-2015-010935
Costa LD, Cura CC, Perondi AR, França VF, Bortoli DS. Perfil Epidemiológico de gestantes de alto risco. Cogitare Enferm. 2016; 21(2): 1-8. https://doi.org/10.5380/ce.v21i2.44192
Leal RC, Santos CNC, Lima MJV, Moura SK, Pedrosa AO, Costa ACM. Complicações materno-perinatais em gestação de alto risco. Rev enferm UFPE. 2017; 11(Supl.4):1641-9.
Salge AK, Castral T, Sousa M, Souza RR, Minamisava R, Souza SM. Infecção pelo vírus Zika na gestação e microcefalia em recém-nascidos: revisão integrativa de literatura. Revista Eletrônica de Enfermagem. 2016; 18: e1137. https://doi.org/10.5216/ree.v18.39888
Silva MG, Vinaud MC, Castro AM. Prevalence of toxoplasmosis in pregnant women and vertical transmission of Toxoplasma gondii in patients from basic units of health from Gurupi, Tocantins, Brazil, from 2012 to 2014. PLoS One. 2015; 10(11): e0141700. https://doi.org/10.1371/journal.pone.0141700
Ministério da Saúde. Diretrizes de estimulação precoce: crianças de zero a 3 anos com atraso no desenvolvimento neuropsicomotor decorrente de microcefalia [Internet]. Brasília: Ministério da Saúde, 2016 [acesso em: 31 mar. 2016].
Ministério da Saúde. Protocolo de atenção à saúde e resposta à ocorrência de microcefalia relacionada à infecção pelo vírus Zika [Internet]. Brasília: Ministério da Saúde; 2016 [acesso em: 31 mar. 2016].
Damasceno ABA, Monterio DLM, Rodrigues LB. Sífilis na gravidez. Revista HUPE. 2014; 13(3): 88-94. https://doi.org/10.12957/rhupe.2014.12133
Domingues RMSM, Szwarcwald CL, Junior PRBS, Leal MC. Prevalência de sífilis na gestação e testagem pré-natal: Estudo: Nascer no Brasil. Rev. Saúde Pública. 2014; 48(5): 766-74. http://dx.doi.org/10.1590/S0034-8910.2014048005114
Siqueira MLBS, Aquino LMM, Silva RA, Mendes SO, Alves SM, Medeiros MO. Prevalencia de infecção pelo Treponema pallidum em gestantes atendidas pela unidade municipal de saúde de Rondonópolis, MT. Biodiversidade. 2017; 16(1): 210.
Abi-Abib RC, Cabizuca CA, Carneiro JRI, Braga FO, Cobas RA, Gomes MB. Diabetes na gestação. Rev HUPE. 2014; 13(3): 40-7. https://doi.org/10.12957/rhupe.2014.12136
Rattner D, Moura EC. Nascimentos No Brasil: associação do tipo de parto com variáveis temporais e sociodemográficas. Rev Bras Saude Mater Infant. 2016; 16(1): 39-47. https://doi.org/10.1590/1806-93042016000100005
Pimentel TA, Oliveira-Filho EC. Fatores que influenciam na escolha da via de parto cirúrgica: uma revisão bibliográfica. Univ Ci Saúde. 2016; 14(2): 187-99. https://doi.org/10.5102/ucs.v14i2.4186
Ferrari AP, Carvalhaes MABL, Parada CMGL. Associação entre pré-natal e parto na rede de saúde suplementar e cesárea eletiva. Rev Bras Epidemiol. 2016; 19(1): 75-88. https://doi.org/10.1590/1980-5497201600010007
Domingues RMSM, Dias MAB, Nakamura-Pereira M, Torres JA, d'Orsi E, Pereira APE. et al. Processo de decisão pelo tipo de parto no Brasil: da preferência inicial das mulheres à via de parto final. Cad Saúde Pública. 2014; 30(Suppl.1): S101-S116. https://doi.org/10.1590/0102-311X00105113
Bello LML, Saavedra PS, Gutiérrez LEG, García JÁH, Serra LM. Características sociodemográficas y sanitarias asociadas con bajo peso al nacer en Canarias. Nutr Hosp. 2015; 32(4):1541-47.
Oliveira RR, Melo EC, Novaes ES, Ferracioli PLRV, Mathias TAF. Fatores associados ao parto cesárea nos sistemas públicos e privado de atenção á saúde. Rev Esc Enferm USP. 2016; 50(5): 734-41.
Oliveira LL, Gonçalves AC, Costa JSD, Bonilha ALL. Maternal and neonatal factors related to prematurity. Rev Esc Enferm USP. 2016; 50(3): 382-9. https://doi.org/10.1590/S0080-623420160000400002
Published
How to Cite
Issue
Section
Altmetrics
Downloads
License
Journal Cuidarte, scientific publication of open access, is licensed under a Creative Commons Attribution (CC BY-NC), which permits use, distribution and reproduction in any medium, provided the original work is properly cited and is not used for commercial purposes.
Any other form of use such as reproduction, transformation, public communication or distribution, for profit, requires the prior authorization of the University of Santander UDES.
The names and e-mail addresses entered in the Journal Cuidarte will be used exclusively for the purposes stated by this magazine and will not be available for any other purpose or other person.
The articles published in the Journal Cuidarte represent the criteria of their authors and do not necessarily constitute the official opinion of the University of Santander UDES.